SAAD provides STAC accredited courses underpinning the knowledge and clinical skills required for the safe provision of conscious sedation in dental practice.
Suitable for dentists, dental nurses, dental hygienists & therapists, for new starters or refreshers.
SAAD is a charity and uses the income from the courses to support sedation research and education.
Attend a SAAD course and be taught by the UK's most experienced teachers of conscious sedation for dentistry!
{slider title="COURSE DATES, FEES & REGISTRATION"}
SAAD offers two face to face weekend courses each year, and a blended course.
Each course consists of theoretical learning and practical skills training.
The blended course is one day online in May, followed by a face to face day in June. The online course can be attended on its own as a refresher, and is available as a recording after the live event for a limited period.
Choose your preferred date and book your SAAD sedation course!
2023
2024
2025
{/sliders}
Further information
Early SAAD
| 1930 - 1950 |
In the early 1930's Stanley Drummond Jackson was a dentist practising in Yorkshire. He was the son of a dentist. In those days dentists largely employed general medical practitioners to provide nitrous oxide based anaesthesia for their patients. Generations of children grew up to know the dread of "gas" at the dentists... As a young dentist Drummond Jackson or ‘DJ' as he became known later, was appalled at the inadequacy and poor quality of general anaesthetic provision for dentistry.
Stanley Drummond Jackson 
 SAAD Logo 'Abolish pain to conquer fear'
SAAD Logo 'Abolish pain to conquer fear'
In a way that would now be considered totally unacceptable but was then completely permissible, Drummond Jackson experimented with new intravenous anaesthetic drugs given by the “venal route” and introduced from Germany and America. By trial and error, he developed a method of intravenous anaesthesia that worked providing fast onset, variable operating time, and quick recovery. DJ was enthusiastic about his technique and over the next seven years he recorded over 8000 successful cases. The Second World War intervened.
Afterwards DJ set up a practice at 53 Wimpole Street, London and continued his use of intravenous anaesthesia. He ran a thriving practice and caught not only the attention of patients wanting oblivion for their dentistry, but also the attention of a group of fascinated medical and dental practitioners. One of these was Dr Henry Mandiwall, a consultant oral surgeon and an accomplished film maker. Together they made a film on venepuncture techniques for general practice. This film was accepted by the British Medical Association and became the first of a series of films detailing DJ's intravenous technique adopted by various teaching bodies.
| 1955 - 1957 |
In 1955 DJ started a study club which rapidly grew and by 1957 the Society for the Advancement of Anaesthesia in Dentistry was born. SAAD’s first president was Mr Alan Thompson, a consultant oral surgeon at Guy’s Hospital, London.
 Alan Thompson
Alan Thompson
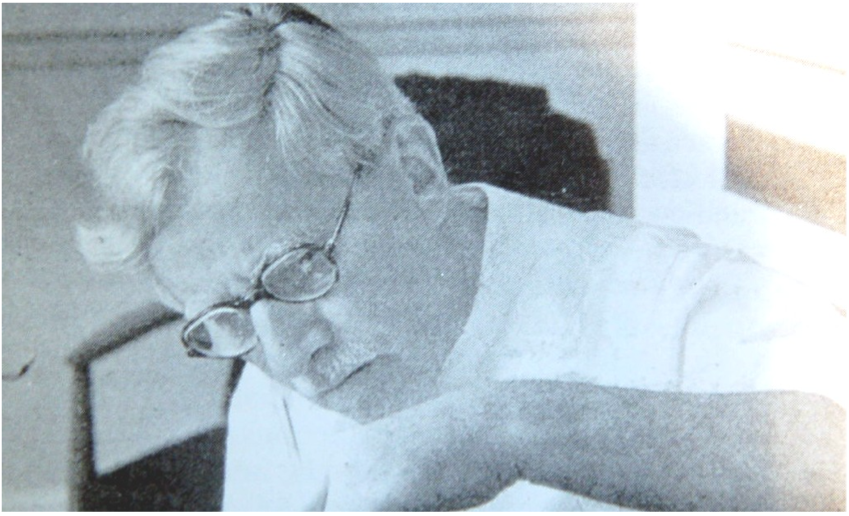
Professor Sir Robert MacIntosh
 It was fortuitous that from the start SAAD attracted the interest of the great and the good. The Society's Trust Deed was drawn up by the Lord Chancellor of England together with a future eminent professor of anaesthesia.
It was fortuitous that from the start SAAD attracted the interest of the great and the good. The Society's Trust Deed was drawn up by the Lord Chancellor of England together with a future eminent professor of anaesthesia.
Robert MacIntosh (later Professor Sir Robert MacIntosh) attended meetings because at the time he was providing anaesthesia for dentistry at a dental practice in Mayfair. Although pursuing a fellowship in surgery MacIntosh needed the money dental anaesthesia brought in. Unwittingly SAAD was to become a catalyst in the academic and clinical development of anaesthesia in the UK. MacIntosh gave an anaesthetic in the Mayfair dental practice to Sir William Morris (of early motor car fame and fortune).
Sir William Morris had previously had an unpleasant anaesthetic experience, but MacIntosh's intravenous dental anaesthetic had changed his view. Morris and MacIntosh became friends and subsequently Morris told MacIntosh that Oxford University had approached him with a plan to endow chairs in medicine, surgery, and midwifery.
MacIntosh persuaded Sir William Morris that to endow a chair in anaesthesia would be both innovative and extraordinary. Ultimately Sir William offered Oxford University, four Chairs including anaesthesia and funding of £1 million.
Opposed to the anaesthetic chair, Oxford University declined so Sir William offered the university £2 million to include anaesthesia on a take-it or leave-it basis.
Unable to resist such a magnificent offer, Oxford University established the first department of anaesthetics in Europe.
Sir Robert MacIntosh became the first Professor of Anaesthesia in Europe and Sir William Morris became Lord Nuffield.
Developing a Scientific Basis
| 1957 - 1966 |
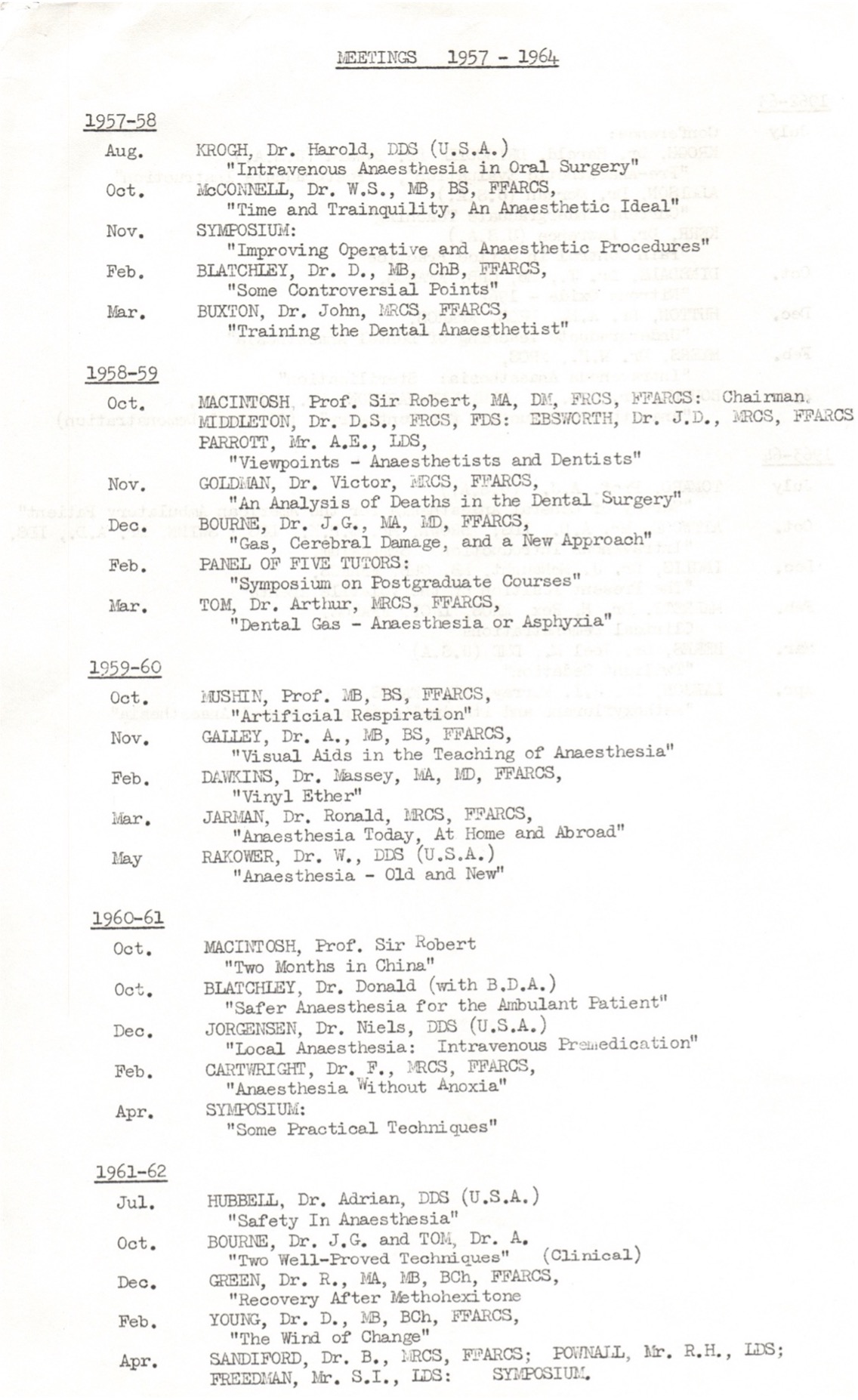
From the very first meeting in 1957, SAAD was heavily involved in the use of intravenous anaesthesia and sedation. From the beginning SAAD had a close association with Guy's Hospital, London and that has continued unabated. Early meetings explored the challenges of barbiturate dosage, laryngeal spasm, aspiration, and the supine position for anaesthesia.
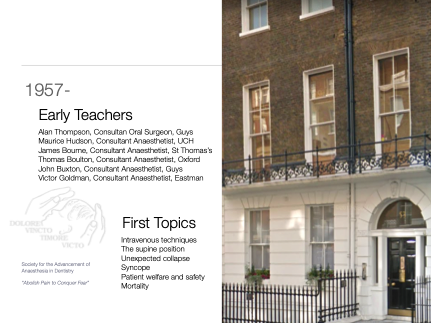
The Society’s policy, which placed patient welfare above all else, was outlined by Mr Thompson at a meeting of SAAD in 1958:
(1) We are agreed that we disapprove of the operator acting also as anaesthetist. At the same time we recognise that exceptional circumstances can arise when such a procedure may be justified.
(2) The policy of the Society is for the overall advancement of anaesthesia in dentistry, for the better care and welfare of our patients. To that end, we do not advocate, or are wedded to, any particular technique.
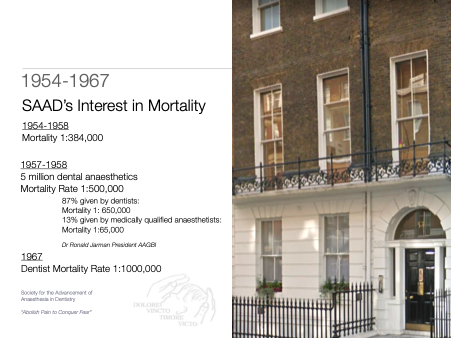
Patient mortality rates were, naturally, an urgent concern. In 1952, a total of 26 deaths out of an estimated 2 million anaesthetic administrations for dentistry purposes were recorded. In 1957 there were 5 deaths, a reduction ‘that it was tempting to ascribe… at least in part, to the increasing use, and safety, of intravenous techniques.’
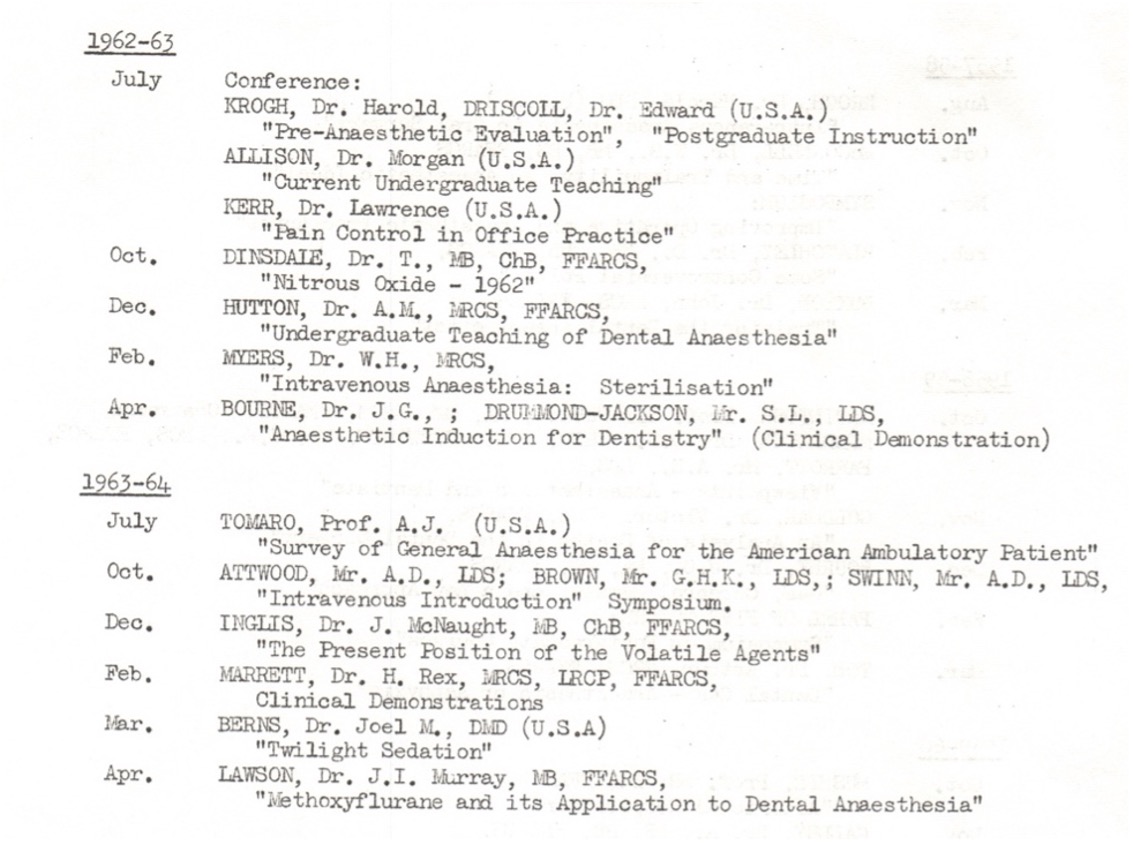
SAAD Diary 1957 - 1966
From the outset SAAD's attitude was clear. The Society had a policy of embracing a range of anaesthetic techniques and formally disapproved of the dental operator also being the anaesthetist. It was agreed that patient welfare was paramount. By 2023 standards, mortality was high with intravenous barbiturates and with these new techniques some career anaesthetists were concerned about selecting the right people to teach how to administer them whether they were doctors or dentists. In the late 1950's it was clear to some that SAAD led the way in the future of intravenous anaesthesia in general and for dentistry at a time when the intravenous route was a minority practice and total intravenous anaesthesia was rare. Meetings were led by Dr John Buxton, a consultant anaesthetist at Guy's Hospital; Dr Morris Hudson, a consultant anaesthetist at University College Hospital; and Dr James Bourne, a consultant anaesthetist at St. Thomas' Hospital, amongst others. Meetings embraced such topics as safety, the causes of syncope and success stories.
Between 1957 and 1960 SAAD was heavily influenced by American and German speakers. There was a particular interest in ultralight anaesthesia and sedation. Intermittent methohexitone sedation and The Jorgensen technique proved to be enlightening for dentists at the time.
In 1959, the technique of intermittent methohexitone anaesthesia was introduced. This was effectively the intravenous drug titrated to effect. As Dr Maurice Hudson, Consultant Anaesthetist and Chairman of SAAD’s sub-Committee on Postgraduate Education, wrote, it was ‘the safest method ever introduced into anaesthetic practice.’ However, even this technique was not entirely free from risk, with the skill of the administrator being of paramount importance.
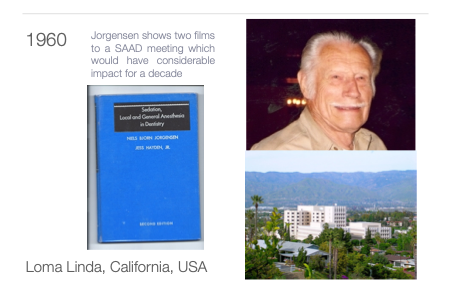
Jorgensen Loma Linda Technique
The ‘Jorgensen technique’, which SAAD began to promulgate from 1960 onwards, owed its name to Professor Neils Bjorn Jorgensen of Loma Linda University, California. Professor Jorgensen visited the Society in December 1960 and outlined the method of intravenous sedation that he had developed. It was not without its problems: effective sedation for a period of less than two hours was difficult to achieve, individual susceptibility varied and could lead to prolonged disorientation or a ‘hangover’ effect of some severity, and – as ever- administration by an inexperienced or heavy-handed practitioner could create its own problems. But it was ‘the first effective step along the road of acceptable dental sedation’, and, given that it allowed for several hours’ work to be undertaken during a single appointment, it was naturally popular.
The first two decades - Update and Jumbo
In 1959 a series of three-day courses were held on general anaesthesia for dentistry. Each course was limited to eight people and took place in the basement of 53 Wimpole Street. The first two days were didactic teaching, and the third day was devoted to clinical demonstrations. As the number of course registrants grew the number of courses went up to eight a year with 24 practitioners on each. In the early 1960’s courses moved to University College London, but the course quickly needed a bigger venue.
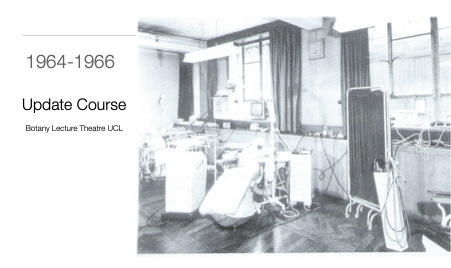
Logistically it became difficult to provide hands on training on an individual basis and practical emphasis was SAAD's modus operandi. This resulted in the development of "table demonstrations" a precursor to the modern rotating seminars of the 1980’s which SAAD still offers today. The Society flourished developing mass training in the so called ‘Jumbo Courses' where up to 240 participants were taught together at University College London.
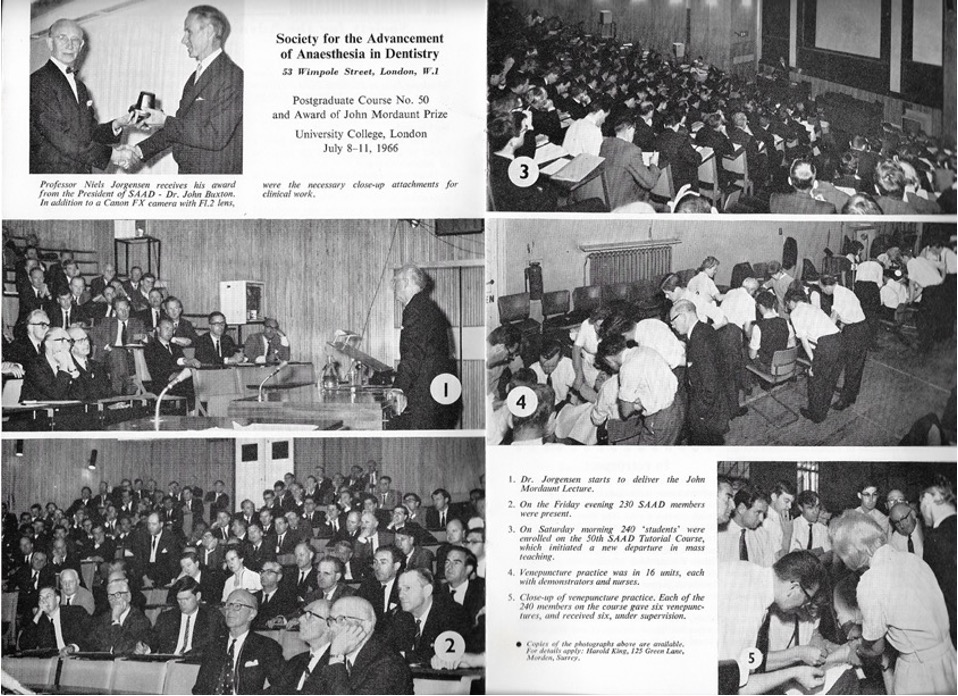
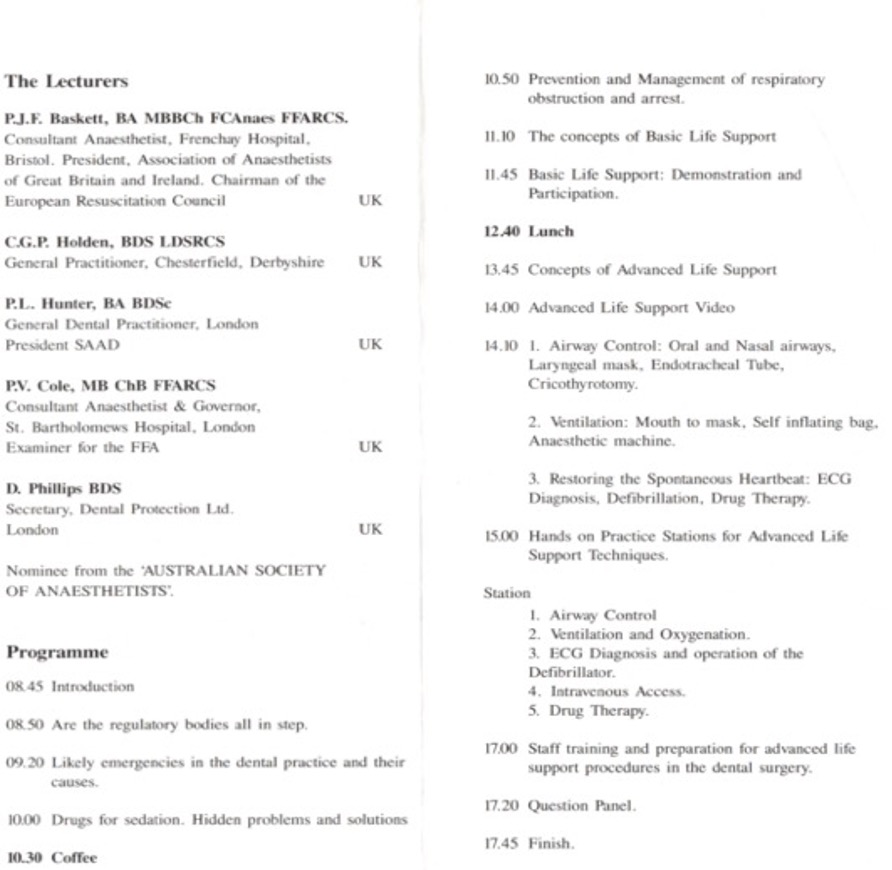
SAAD Course - July 1996
The first “Jumbo” course took place on 9th July 1966 at University College London, with 240 students undertaking and receiving two cannulations on all three days of the course. Four fully equipped dental surgeries were installed in the College gymnasium and a different technique demonstrated in each. The first demonstrations in this “four-ring circus” covered advanced conservation under Jorgensen sedation; oral surgery under diazepam sedation, and intermittent methohexitone anaesthesia. “The Society makes no attempt to justify such mammoth courses on the basis that they are good as personal tuition,” a subsequent report stated. “However,… there are many hundreds of dental graduates, ill-trained in anaesthetics, who are at present administering traditional methods under conditions which are far from satisfactory. And whatever amount of training they have had, few have been given the basic groundwork of safe practice which is so essential for the welfare of patients under all conditions.”
The drawbacks of the Jorgensen technique of extended sedation, long recovery, and potential hypoxia and hypercapnoea were not inconsiderable. The commercial availability of diazepam as intravenous Valium arrived. In 1968, a SAAD symposium was devoted to the dental uses of the drug, although at the time its makers, Roche, objected to its use outside hospitals. However, its advantages were clear: sedation could be of shorter duration and its effects more controlled, the patient remained co-operative, and the amnesia that followed ‘could be exploited in the fearful patient to promote a return for further treatment without terror.’ The drug’s safety determined, and Roche’s objections notwithstanding, SAAD began to promulgate its use.
From the following year, 1967, participants were formally required “to have experience of the administration of anaesthetics and the handling of emergencies”. Those who did not possess the latter were directed to their local branch of St John Ambulance or the Red Cross. As Peter Sykes observed, this is particularly striking because it was not until 1989 that the General Dental Council decreed that “all dental practitioners and their staff should be competent in basic resuscitation”[1]. Indeed, it was the pressure put on the GDC by SAAD through Peter Sykes and Gerry Holden, both elected members of the GDC, that led to it adopting this stance.
Safety was, as always, SAAD’s governing principle, and by 1967 10% of all UK dentists had attended a SAAD course.
The development of teaching from the beginning to our modern society today traces a record of the challenges of teaching large numbers of doctors and dentists new clinical skills and the provision of safe and comfortable care for patients in constantly changing political circumstances. Some doctors and dentists openly disapproved of SAAD's initiative.
SAAD grew rapidly as did the practice of intravenous anaesthesia in dentistry. By 1967 membership was 2000 and 10% of dental practices in the UK provided intravenous anaesthesia. This rapid spread led to alarm by an increasing number of dentists and anaesthetists.
The Supine Position
Another milestone in the history of SAAD came with the development of the first supine electrically driven dental chair. Until the 1960s in Britain, practitioners traditionally stood behind and bent over their patients, who were seated upright in a chair. To operate the footswitch of the dental drill, the dentists were required to stand on one leg.
SAAD had a long debate about syncope on induction of sedation and the “sit up and beg” traditional dental chair was seen as cumbersome and not fit for purpose for sedated patients.
In 1967, an American dentist, Dr Daryl Beach, visited the Society to expound the virtues of the supine technique (ease, efficiency, and comfort chief amongst them). Beach had designed his own ‘Spaceline’ unit, a flatbed “chair” that incorporated suction, compressed air, and hand instruments into its housing, and it was this that inspired SAAD member and future President Dr Gerry Holden to develop a reclining chair to accommodate SAAD’s intravenous techniques. His ideas, and the demand from ever-increasing numbers of practitioners, proved formative in the design and development of dental units. Importantly, these units recognised the increasing role of dental nurses, who now required their own instruments. Functions were therefore divided or incorporated into special mobile units to best allow both operators to perform their respective duties.
The SAAD-developed chair also converted to a bed by electric power, whilst constantly maintaining the position of the arm for the administration of intravenous drugs. Without this innovation, the treatment of patients in the supine position would not have developed so quickly. It would be ten years until UK teaching institutions widely adopted the supine position.


The Operator-Anaesthetist
| 1971 |
In 1971, a government proposed ban on the operator-anaesthetist in dentistry brought what had been a long-running debate to the fore. This had particular significance for SAAD, since a ban ‘would have effectively abolished the intermittent methohexitone technique on which most of SAAD’s teaching was based, because only rarely was it practicable in general dentistry to obtain the services of a separate anaesthetist; however desirable this was admitted to be. Equally significant was that ‘patients faced being denied a safe and effective pain and anxiety control technique’.
SAAD produced a booklet entitled “Treachery” highlighting politically motivated rather than safety motivated proposed regulatory action.
Peter Sykes commented: Along with The British Dental Association, SAAD took on the Government …… “Treachery” was sent to every Member of Parliament detailing both the sacrifice of basic rights of patients and professional freedom of doctors and dentists and the potential loss of invaluable years of progress in pain control. Members of Parliament agreed - SAAD and the BDA won.
The almost invariable presence of a SAAD Council member on The General Dental Council was a further check and balance when it came to the regulation of anaesthesia, conscious sedation, and resuscitation. Particularly notable in this respect was Dr Gerry Holden (SAAD President 1975-1980), whose 1978 definition of conscious sedation for The General Dental Council was developed with Professor Sir Paul Bramley an oral surgeon at Sheffield University. That definition was adopted by The General Dental Council and is still widely accepted, almost unchanged, today.
Litigation
SAAD has never avoided the tensions and professional differences between doctors and dentists over who should give what to whom, where and when.
Methohexitone anaesthesia became the centre of a libel case that led to already existing tensions between SAAD and some sections of the medical anaesthetist community coming to a head. In 1969, the British Medical Journal published a paper on the use of intravenous methohexitone for conservative dentistry. The technique, and Drummond-Jackson himself, were both condemned, although the paper’s authors had not followed the technique promulgated by SAAD. When DJ’s request that the BMJ publish a statement of withdrawal was declined, he sued for libel.
What followed was the longest libel action in British legal history for fifty years. Concerned at its length, the presiding Judge, Mr Justice Acker, finally advised that the case be concluded, and that each party ‘exonerate the other from any ulterior motive’.
| 1979 |
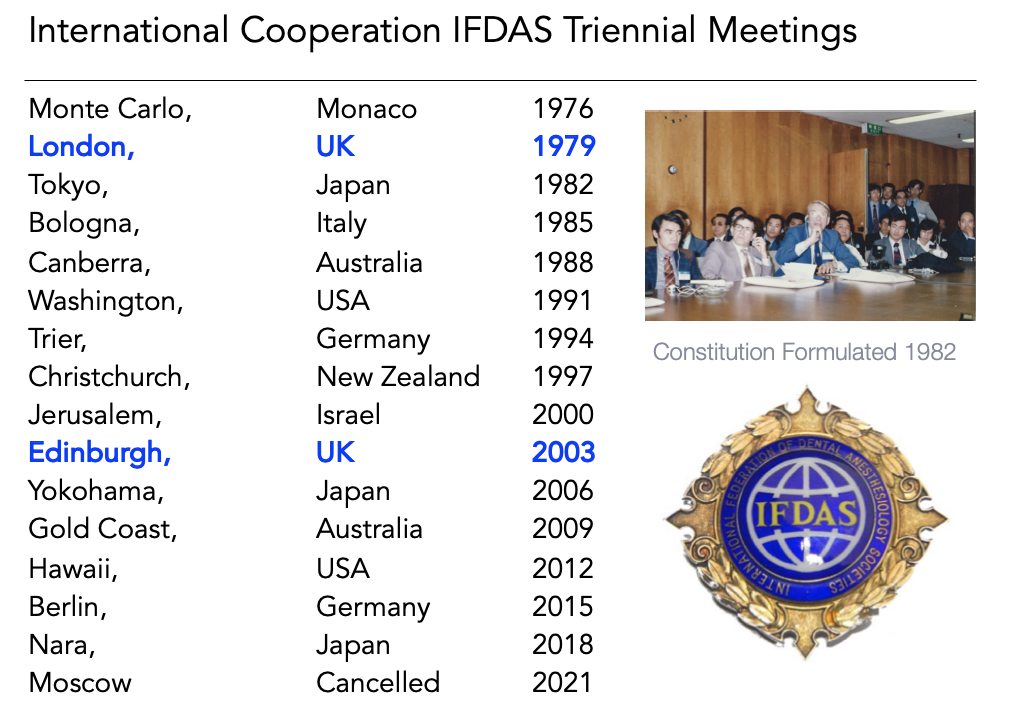
In the 1970’s SAAD had continued interest in developments in other countries and recognised the benefits of international cooperation. The society was keen to establish a formal international organisation. To that end SAAD offered to host an international meeting in London in 1979. Led by Dr Gerry Holden a general practitioner and member of The General Dental Council, who was SAAD’s president at the time. SAAD 79 was a huge success both academically and socially and it set the scene for triennial congresses for decades later. The meeting was considered important enough for the government to host a formal government reception at The Lancaster Hotel, St James’s.
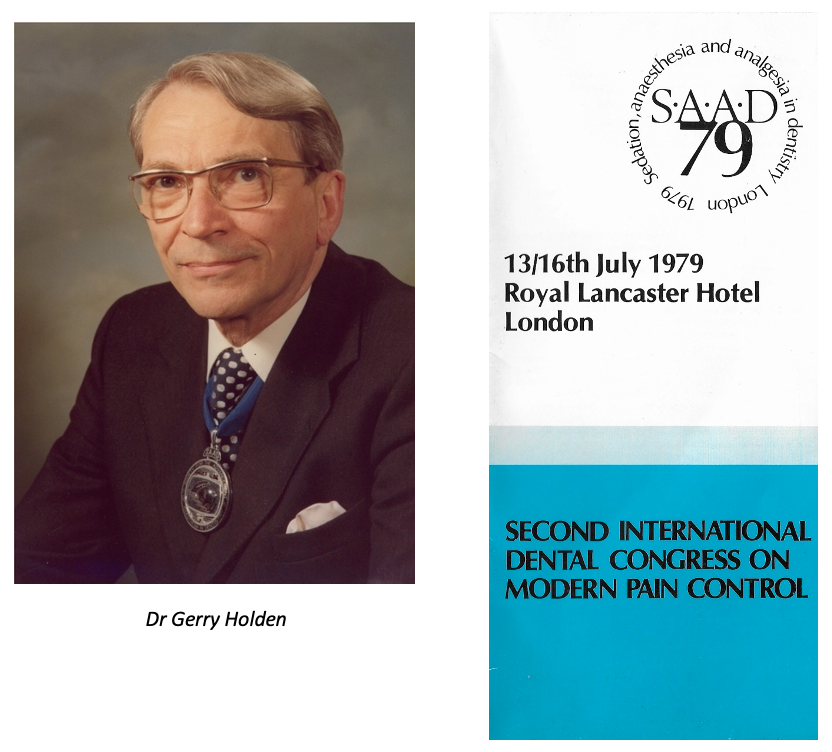
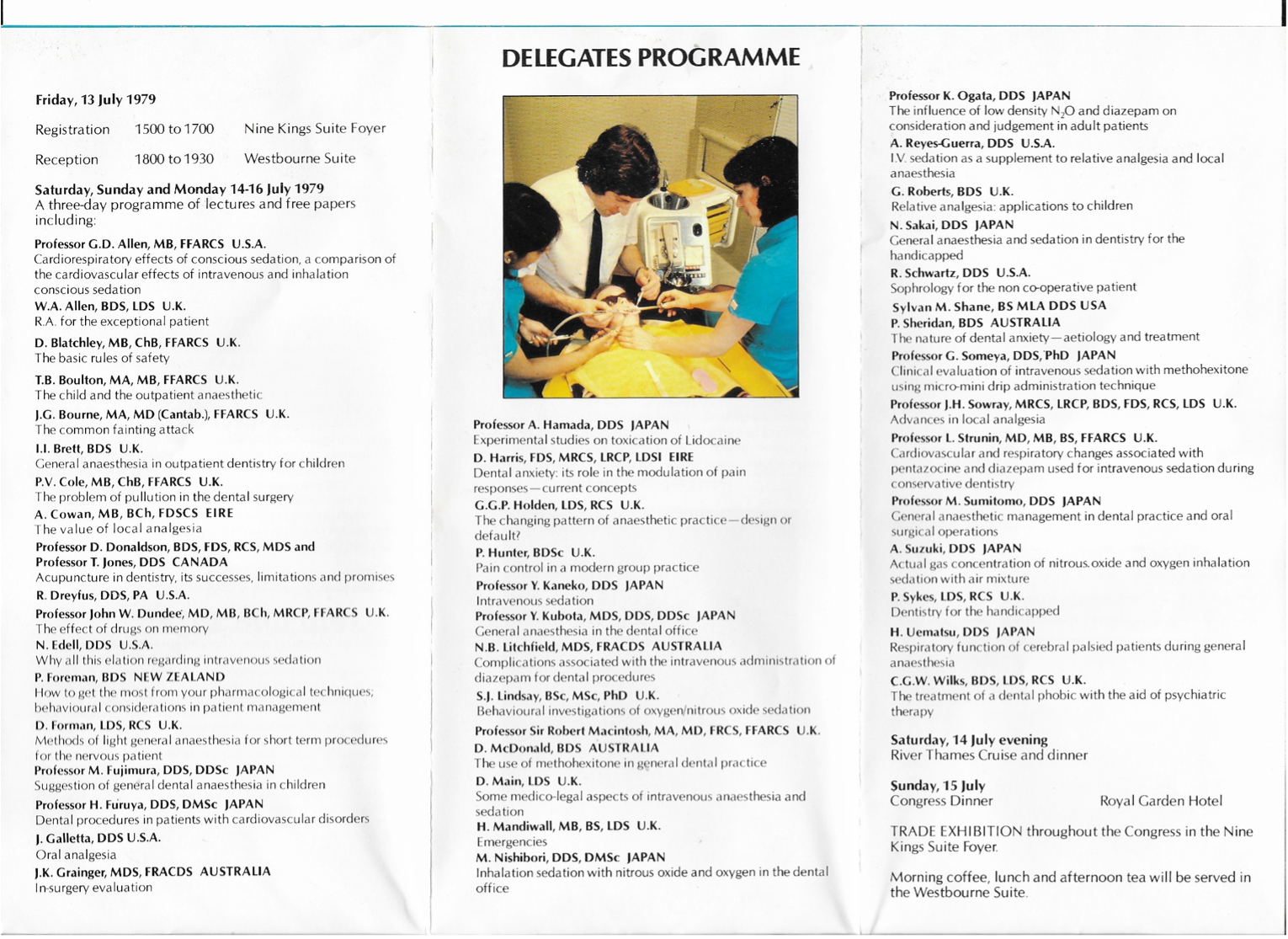
At SAAD 79 the foundations of a formal international federation were conceived which was to be formalised in 1982 at a subsequent congress in Tokyo, The International Federation of Anaesthesiology Societies. IFDAS formed an important conduit for developing and sometimes even harnessing national aspirations particularly in relation to guidance and regulation. The Federation appointed as its first Secretary General, SAAD Council member, Dr Peter Sykes. IFDAS flourished and gained new membership quickly and SAAD continued to fly its flag on the international stage at each of the triennial conferences.
It was clear to most that doctors and dentists had to co-operate and collaborate in the provision of pain and anxiety control for dental patients, but it took a generation to heal the wounds of litigation and both professions viewed each other with some suspicion. Thankfully for SAAD, there were dentists and anaesthetists who saw beyond this narrow issue and Dr Thomas Boulton a consultant anaesthetist from Oxford and Reading and soon after President of The Association of Anaesthetists drew the professions together during his presidency of SAAD in 1980.

The need to teach both sedation and general anaesthesia in a structured way to ensure safety - especially outside of a hospital environment - was becoming increasingly evident to the dental profession. As a result, the medical and dental faculties of the medical royal colleges together with the General Dental Council produced guidance in 1981 with a view to training dentists in general anaesthesia. Several university training/service posts were created and many of these ‘Wylie Trainees’ subsequently went on to SAAD teaching posts, including Dr David Craig and Dr Christopher Holden. At that time some universities were providing a group of young dentists with formal training in general anaesthesia for dentistry during a full time postgraduate in-service training course. Most of these joined SAAD and lacking the baggage of recent history began to renew progress. After the legal case the Society continued to develop by insisting on academic competence, clinical excellence, and appropriate training pathways.
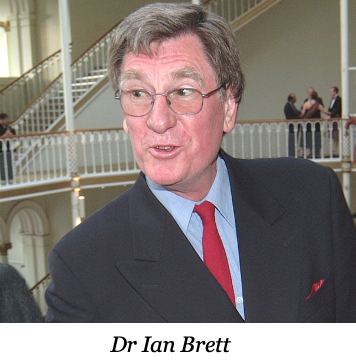
The early 1980s were financially difficult for the Society and but for a new and firm treasurer in Dr Ian Brett SAAD may well not have survived. Ian Brett was a general practitioner in Wimpole Street having taken over Stanley Drummond Jackson’s practice with The Lord Colwyn. Always unassuming Ian Brett coaxed the finances through good investment and wise spending control. This disciplined approach cemented the continuation of teaching until the late 1980’s when one day update courses started. Those courses turned around SAADs financial fortunes for decades to come.
In the 1980's the mainstay of SAAD's training remained two or three day courses with a large practical element. This became known as the "Main Course". During this time SAAD courses moved between the Eastman Dental Hospital, the Whittington Hospital, and the Royal Free Hospital at Hampstead, all necessitated by fluctuating numbers of course participants.
From 1980, SAAD began to promote inhalation sedation (also known as inhalational sedation, Relative Analgesia or RA). This psychosedative technique was imported from the USA and represented a very safe form of mild sedation, relying on maximal suggestion and minimal amounts of nitrous oxide with oxygen. Not to be confused with Entonox it was a hypnotic technique. This proved to be a good alternative for children who were less suited to intravenous techniques. In the mid-1980s, the need to improve the characteristics of intravenous diazepam (Valium) was recognised and a watershed in sedation was about to occur. Although when titrated diazepam produced moderate sedation, its effects were not totally predictable in teenagers who could become tearful and agitated from paroxysmal effects.
| 1984 |
SAAD began to teach the use of intravenous Midazolam (Hypnovel / Versid) in preference to Valium in 1984/1985, with its training becoming more didactic in nature consequently, due to the potency of Midazolam over other benzodiazepines.
For a time the main course moved to the practice of Dr Peter Hunter in Acton London. Peter Hunter was a forward-thinking Australian dentist whose practice was technologically advanced in equipment, ergonomics and early computerisation.
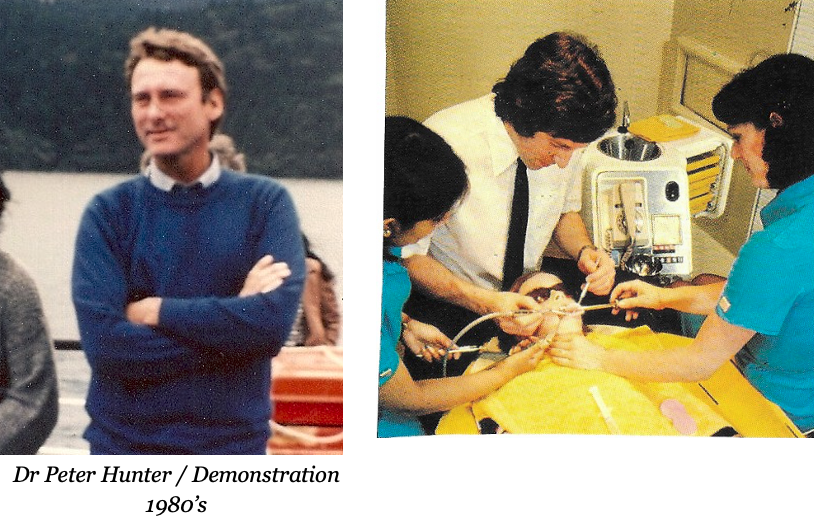
The facilities necessitated a rotation of small groups experiencing up to eight clinical cases a session. Peter Hunter always charismatic, and never still quickly realised the benefits of this style of training and decided to develop SAAD's seminars.

The course organisers during this time included Dr Brian Swinn a general practitioner from Southampton, and Dr Douglas Stewart who later emigrated to Australia to become an associate professor in dental sedation in Sydney. Following a move to St Bartholomew's Hospital in London, SAAD courses settled there until 2004. A new drive by sequential course director kept “The Main Course” as it had been known contemporaneous and a professional leader. The course developed into “The National Course in Conscious Sedation for Dentistry” reflecting SAAD as the largest postgraduate teaching organisation in this field in the UK.
| 1986 |
SAAD produced its first guidance document, Guidelines for Physiological Monitoring of Patients during Dental Anaesthesia or Sedation, in 1986. SAAD Council insisted that this should guidance whose goal was achievable by all but underpinned by a minimal standard. A working party was established chaired by Dr Peter Cole a consultant anaesthetist at St Bartholemews hospital, London, and included the youngest and oldest members of council. So it was authored jointly by SAAD dentists and anaesthetists, combining both academic opinion and the opinion of experienced clinicians in primary and secondary care.
| 1987 |
SAAD’s educational mission became the teaching of conscious sedation and life support as opposed to general anaesthesia. Recognising the need for sedation courses to be consistent in content and presentation wherever they were offered, SAAD introduced the National Course in Conscious Sedation for Dentistry in 1987. The format of lectures and live patient cases continued, these being delivered by a growing faculty of dentists, doctors, and anaesthetists. As Christopher Holden comments: “SAAD became synonymous with simple, safe, titrated techniques that kept the patient sedated and comfortable but distant from the oblivion of general anaesthesia.”
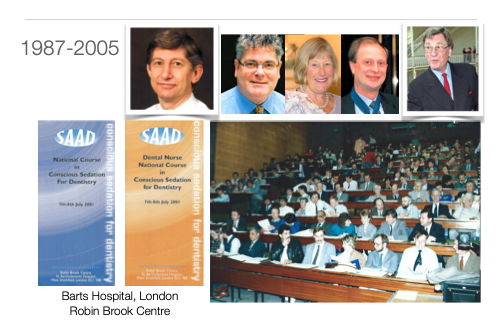
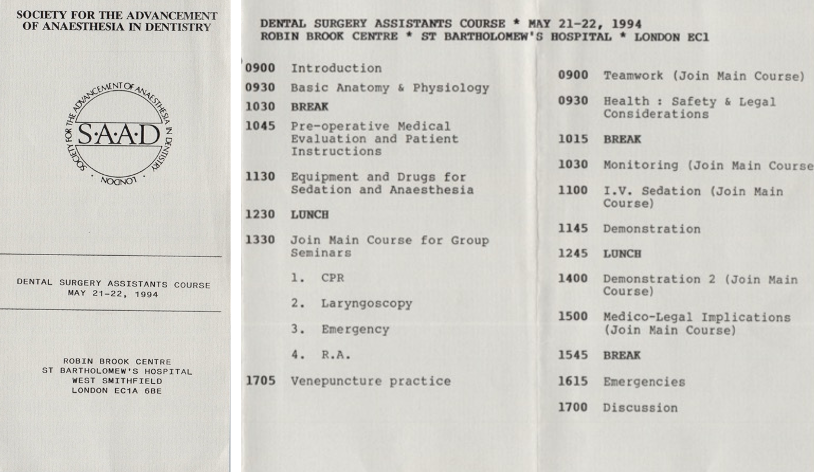
1987 also marked the beginning of the first course specifically designed for dental nurses, filling a gap in training identified by Dr Ian Brett. In fact, it had been proposed as early as 1965 that SAAD should offer a training course to dental nurses, but a lack of willing tutors prevented the idea from coming to fruition. The new course was first delivered at 53, Wimpole Street, London, Ian Brett’s practice. Peter Sykes commented that “represented one of the few specialised sources of training in anaesthetic nursing available to the dental nurse.”
During these years attendance at these courses was built as SAAD pushed towards standardised training. The plural nature of the faculty drew on the varied experience of university teachers, general dental practitioners, anaesthetists, and general medical practitioners.
The Society was beginning to develop a more structured training. The courses were relaunched as the National Course in Conscious Sedation for Dentists and Dental Nurses. Both programmes were fully audited continuing professional education programmes offered on a national scale. The new style training and the travelling seminars overcame SAAD's financial difficulties, and the society became financially secure.
Updates and Lifesavers
| 1988 |
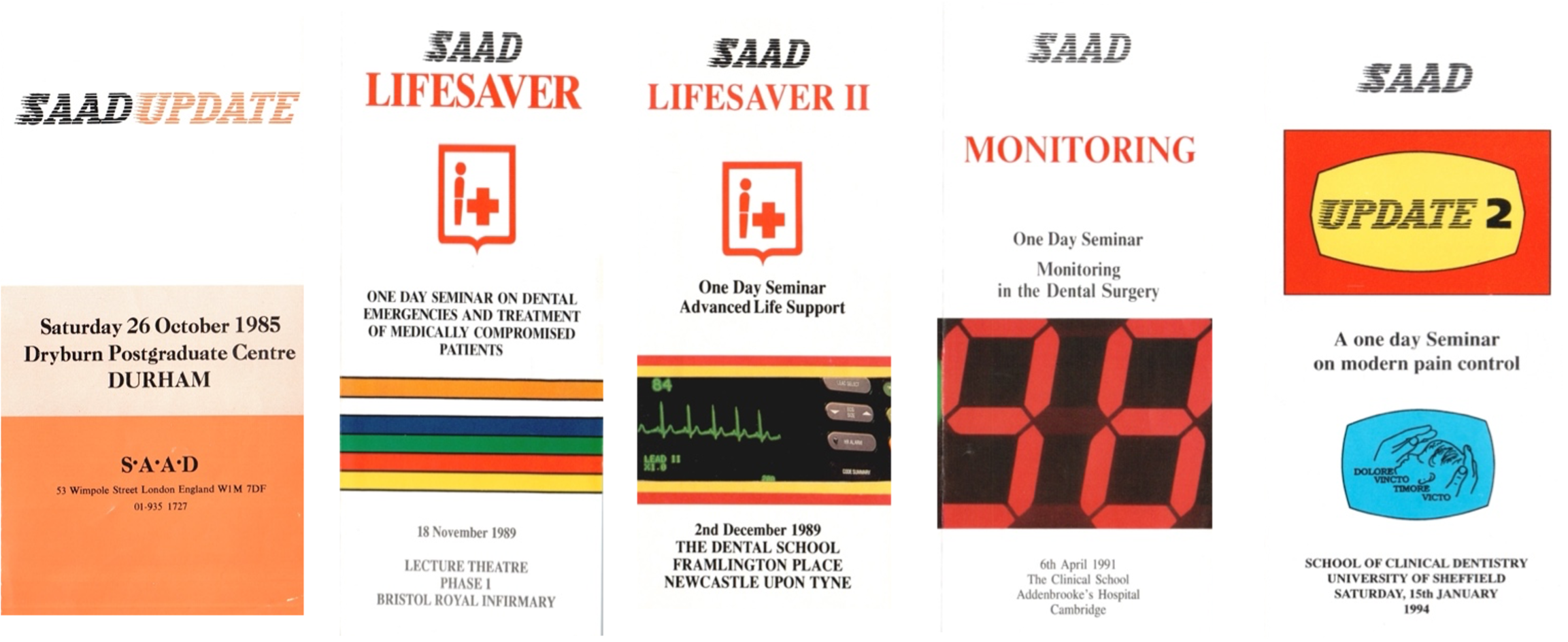
With Dr Peter Hunter's enthusiasm and organisational skills SAAD was one of the first professional groups to develop the "travelling road show" where a diverse group of experts would travel the country to provide the same programme in one or two days. Seminars were titled SAAD Update, Monitoring, Lifesaver I, Lifesaver II, and Update 2. The format was short, punchy lectures followed by rotating practical seminars. The faculty small but dedicated and delivered 59 of these courses.
The Lifesaver courses were amongst the most successful courses run by SAAD. Lifesaver I, the first nationally available CPR course directed at dentists, was attended by over 6000 dentists – more than one third of all UK dentists. Eight years later, in 1996, Lifesaver II was rolled out for the purposes of teaching Advanced Life Support.
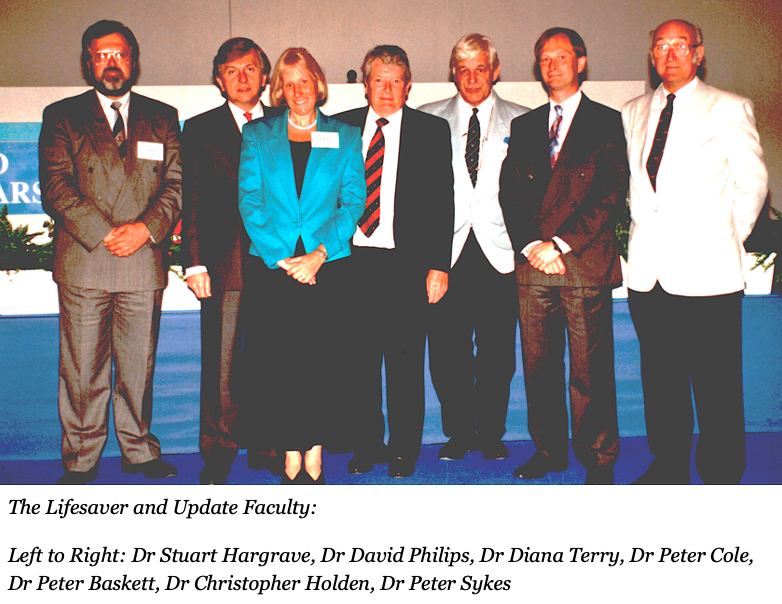
SAAD led the way in the late 1980's and early 1990's with resuscitation training for dentists. Although a requirement of the General Dental Council, resuscitation and sedation complication rescue capability was varied both within dentistry and medicine. Training was generally difficult to obtain and largely theoretical. SAAD took up the challenge. This was enthusiastically supported by Dr Peter Baskett a consultant anaesthetist from Bristol who had a background of military anaesthesia and life support. At The Frenchay Hospital, Bristol he trained the first ambulancemen to become what we now know as paramedics in 1969. Peter Baskett became President of The Association of Anaesthetists of Great Britain and Ireland and president of the Faculty of Anaesthetists of The Royal College of Surgeons England led the education taught on the seminars.
| 1995 |
Occasionally SAAD also provided short courses with a reduced faculty both in the UK and in several other countries including Germany, France, Belgium, and Zimbabwe amongst others. Wherever it benefitted patient safety SAAD worked with other organisations such as The Association of Resuscitation Training Officers (ARTO) to further training.

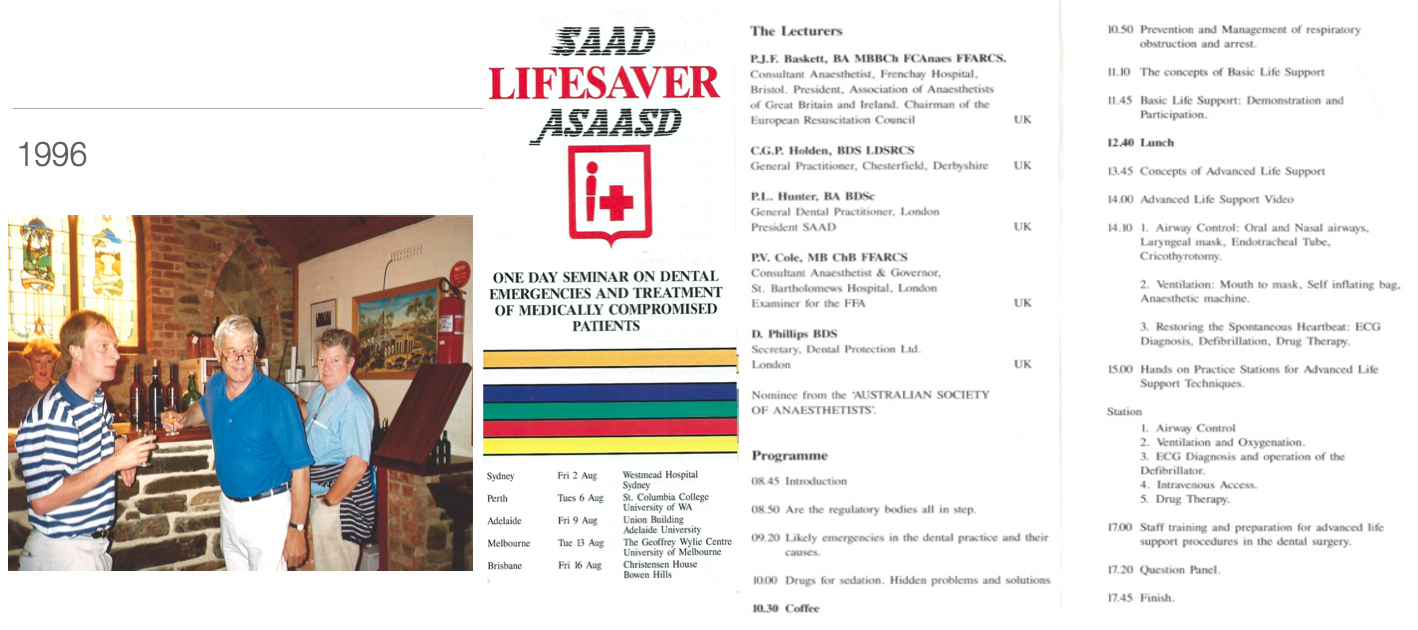
| 1996 |
The LifeSaver seminars were so successful that the format of LifeSaver 1 and LifeSaver II was exported in its entirety to Australia. SAAD’s then secretary, the Australian-born Peter Hunter, thought that the course could also be successful in Australia. Although the SAAD council was more than concerned that there might be some resentment of foreigners perceived to be importing “knowledge”, the course was run in all the major cities of the Australian continent in just 17 days. It was a resounding success in participant numbers. SAAD’s hosts in each city were generous and welcoming. As Christopher Holden remembers, “Those of us teaching on this programme spent more time on aeroplanes than teaching.”
| 1997 |
By 1997 SAAD's teaching had transformed from a decade previously and the 40th Anniversary Programme concentrated on new sedative drugs, undergraduate teaching, and the role of dental nurses. The Society was beginning to develop a well-structured training pathway. The courses were relaunched as the National Course in Conscious Sedation for Dentists and Dental Nurses. Both programmes were fully audited continuing professional education programmes offered on a national. During the next five years the society became comfortable reaching out to all specialties within dentistry.
| 1999 |
In 1999 the SAAD “Part 2” course came into being. Developed at Guy’s Hospital by Dr David Craig, its purpose was to help nurses prepare for the National Examining Board for Dental Nurses (NEBDN) Certificate in Dental Sedation Nursing. This finally embedded dental team training as a concept SAAD continues to this day.
As numbers grew it was increasingly challenging to provide teaching heavily reliant on live case presentation a feature of SAAD’s training since inception. The arrival of digital media allowed a streamlining of teaching and less reliance on the logistically difficult live case presentations.
| 2001 |
In 2001, David Craig, who led the Department of Sedation and Special Care Dentistry at Guy’s Hospital, became SAAD’s course director and introduced fundamental changes. These included reducing the National Course from three (labour-intensive) days’ duration to two and a phasing out of its more improvised elements (a portable dental chair constructed by Dr Ian Brett was honourably retired at this time). Live demonstrations of conscious sedation ceased, and procedures were put in place to ensure that the various components of the course – including registration and the provision of equipment and supplies – ran more smoothly.
After many years, SAAD’s courses found a new home in November 2005 when they moved from Barts to Queen Mary University of London. QMUL offered better facilities and the capacity to accommodate ever-growing numbers of participants: in 2001, 70 dentists and 50 dental nurses were booked on the November National Course at Barts; by 2020 enrolment figures were around 100 dentists, 80 nurses and up to 10 therapists/hygienists.

Queen Mary University of London
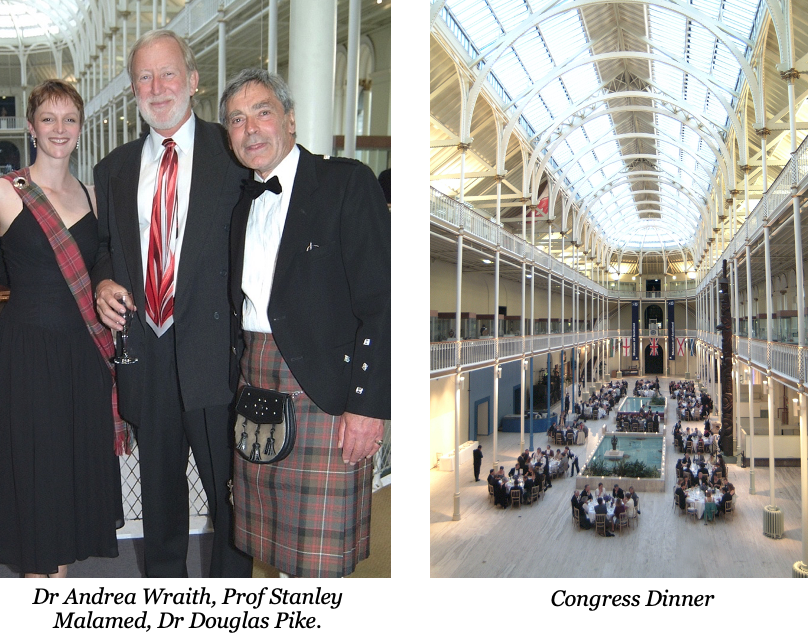
Dr Christopher Holden During the Presidency of Dr Christopher Holden (2000-2003), SAAD continued to develop organisationally, and, for the first time, job descriptions were introduced for all Council members as the formalised structure of the charity was developed. Along with other SAAD Council members Christopher had a background of council and committee membership of The Association of Dental Anaesthetists, Dental Sedation Teachers Group, and subsequently Academy of Medical Royal Colleges and multiple groups providing professional guidance for sedation. As a member of the Advisory Board of Dental Protection the dental arm of The Medical Protection Society his interest was reflected in a period promoting demonstration of safe and justifiable sedation practice. After a series of experiences as an expert witness Christopher Holden persuaded SAAD Council the need for national standards in conscious sedation for dentistry. Subsequently SAAD published a comprehensive guidance document that was effectively the first “steps to take” direction to SAAD members providing dental sedation. This was swiftly seen by the Department of Health as a useful tool for patient safety. It then commissioned its own standards document. That in turn led to a series of contemporaneous standards documents over the following decades. SAAD became a respected stakeholder in these. Christopher Holden said “The diverse professional background of SAAD Council members dedicated to patient safety and leading the standards setting continuum belied any view that SAAD members were simply enthusiasts” A number of regional ad hoc courses contributed to the centralised teaching including ‘First Response', a course on management of medical emergencies using advanced simulation techniques, led by Dr Diana Terry of the Resuscitation Council UK. The “First Response” course introduced in 2000 was particularly significant– and it could not have been timelier. In July 2000 a Department of Health Review Group concluded that: “All dental practices must have the appropriate equipment and drugs to deal with emergencies or the collapse of patients. The staff must be trained in coping with such emergencies. All members of the dental team must practice resuscitation together at regular intervals.” A landmark in SAAD history came in 2003, when SAAD played host to the International Federation of Dental Anesthesiology Societies’ Congress. It was the second time in 30 years that this honour had fallen to SAAD (which had after all played a key role in its formation), and the 10th IFDAS Congress. To appeal to as broad a range of international delegates as possible, as well as to reflect SAAD’s status as a UK-wide association, Edinburgh was chosen as the location. Driven by Christopher Holden, Douglas Pike, and Andrea Wraith the congress was seen as an opportunity to show SAAD at its best. SAAD council approved the underwriting of the venture, a decision that circumstances could have caused the society to take a hard financial hit. Unfortunately, the timing proved unpropitious, as Douglas Pike reported at the time: “Holding a big international conference just after the Iraqi war and at the height of the scare surrounding the SARS virus was challenging. The aim was to give those delegates that did brave the danger in the skies a conference to relish and remember. In the event that was exactly what the participants got.” The opening reception was held in Edinburgh Castle, with former SAAD President Lord Colwyn opening the Conference. Lord Colwyn was at the time still practising dentistry in London and, as the SAAD summer newsletter noted, he ‘As it happens… sedated two patients the day before departing for Edinburgh.’ IFDAS 2003 attracted 449 delegates, of which 234 were from the UK. The international delegates came from 28 countries, including China, Mexico, Nigeria, Russia, South Korea, and Sri Lanka. There were 75 speakers, and 161 workshops. Professor Stanley Malamed of The University of California gave the opening address, and in the words of Douglas Pike ‘set the scene for the conference by highlighting the balance between patient safety and fulfilling patient expectations. In a word, education really is the key to pain and anxiety control for dentistry. Education not regulation was the theme that emerged from session after session.’ The Conference closed with the Presidential Scottish Banquet in the Great Hall of the Royal Museum of Scotland, complete with haggis, neeps and tatties and a Ceilidh. It was a memorable occasion (to the relief of SAAD Council, which had invested seed funding of nearly £20,000), and one that also saw the installation of Christopher Holden as President of IFDAS for a term of three years (2003-2006). David Craig was SAAD’s Course Director from 2001 until 2019. He became President of SAAD in 2003. The most important business occupying SAAD Council at the start of his Presidency was the new Trust Deed and Constitution. Several Council members had expressed concern that the existing deed no longer met the requirements of a modern charity. President-Elect Diana Terry led Council’s deliberations on this matter and, with the help of Bill Hamlin, Jason Leitch and Hugh Lyons, extended the remit to include the long-ignored question of professional indemnity for members who advise practitioners or teach on SAAD’s postgraduate courses. In light of the increasing number of inspections being carried out by Primary Care Trusts of practices offering dental treatment under conscious sedation, Council members Derek Debuse and Andrea Wraith produced draft guidance designed to encourage inspectors to seek appropriate and relevant information in an update of The SAAD Evaluation Scheme. The resulting SAAD document contained a checklist along with accompanying notes and references. It was the origin of many similar checklists. Around this time there was much discussion about the role of the so called ‘Advanced’ sedation techniques. In 2003 SAAD’s Annual Symposium, held in the Council Chamber of the General Dental Council, focussed on this topic; many of the comments and suggestions were subsequently incorporated into the SAAD National Course programme. In April of the following year, SAAD and the Faculty of Dental Surgery of the Royal College of Surgeons of England jointly presented a ‘Masterclass on Conscious Sedation’ to a capacity audience at Lincoln’s Inn Fields. The symposium covered Basic and Advanced techniques, education and medico-legal issues. The Society maintained its position as the UK’s largest provider of postgraduate sedation education. The National Course in Conscious Sedation for Dentists and Dental Nurses was highly successful and heavily over-subscribed. The course programme continued to focus on the most useful and widely used ‘Basic’ sedation techniques whilst providing an introduction to ‘Advanced’ options. David Craig’s presidential reports to SAAD Council and at the AGMs all pay tribute to SAAD's Executive Secretary Fiona Wraith’s tireless support for all SAAD’s activities during, what had turned out to be, a very busy three years. The SAAD Digest and Newsletter, edited by Andrea Wraith and Jason Leitch, continued to be an important part of SAAD’s communication with the membership. In 2004 all members received a short questionnaire relating to the future of SAAD’s publications. The Royal Society of Medicine had been the regular meeting place for SAAD until 1981. SAAD returned to the venue for the annual symposium in 2004. This relationship has continued annually to date. The RSM has provided both a welcome sense of continuity and excellent facilities for delegates, including accommodation for those travelling to London or wishing to In 2004 SAAD Council signed a collaborative agreement with GKT Dental Institute (GKTDI) to establish the SAAD/GKT Visiting Professorship in Pain and Anxiety Control for Dentistry. Peter Milgrom, Professor of Dental Public Health Sciences at the University of Washington in Seattle, with a long-standing interest in the management of dental anxiety was appointed to this SAAD funded post for a period of three years. The negotiations between SAAD and GKTDI were led by Douglas Pike and Nairn Wilson, Dean of GKT Dental Institute. David Craig, Head of Sedation and Special Care Dentistry at Guy’s and St Thomas’ NHS Foundation Trust agreed to accommodate Peter Milgrom in his department. In 2004 SAAD was invited to contribute to the BDA Conference in Bournemouth. Past President Christopher Holden organised a panel of speakers which included Michael Wood, Jason Leitch, Nigel Robb and David Craig. The 2004 Annual Symposium, organised by Carole Boyle and Barry Devonald, explored the impact that Primary Care Trusts were exerting on the provision of conscious sedation in primary care. The subject had had been proposed by Douglas Pike. Hugh Lyons (Treasurer) suggested that it should be free-of charge to current SAAD members Moving SAAD’s central office to the home of the Association of Anaesthetists of Great Britain and Ireland (AAGBI) at 21 Portland Place took place at this time and was a great success. Not only did we have Busola Oguntula from the AAGBI looking after our administrative affairs but we acquired a first class venue for meetings in Central London. Early in 2004, SAAD Council agreed that it would be appropriate for all Past-Presidents to receive a miniature medal based on the SAAD Presidential chain of office. These were struck by Thomas Fattorini of Birmingham and presented at a dinner held at the AAGBI. SAAD became an incorporated (as opposed to unincorporated) Charity on 1st January 2005. As an incorporated charity, SAAD could retain funds and enter contracts; trustees also benefited from the protection afforded to directors of a company. Documents were produced to detail the charitable objectives of SAAD and to ensure that it complied with legal requirements. The Board of Trustees (the new name for SAAD Council) agreed a new trust deed and Constitution. These replaced the old trust deed and original constitution that had been drafted by the Lord Chancellor of England, but which no longer met legal and practical requirements of a modern charity. In 2005 Christopher Holden led a complete redesign of the SAAD website - the Society’s gateway for anyone seeking postgraduate training or interested in wider involvement in pain and anxiety control. For many years, SAAD’s National Courses had been held at the Robin Brook Centre at Barts’ Hospital but in 2005 we were given notice that the buildings were to be refurbished and the range of accommodation we required would no longer be available. SAAD Council accepted the Course Director’s proposal to relocate all future National Courses to Queen Mary University of London (QMUL) in Mile End Road. This change of venue and the increasing number of applications for the three National Courses run each year kept the Course Director and Course Organisers Derek Debuse and Toni Philpot extremely busy. From 2006 all courses were run at QMUL. Dr Diana Terry, a consultant anaesthetist from Bristol became SAAD’s first female president in September 2006. Understanding that SAAD was respected for teaching but lacked a scientific journal of standing Diana Terry persuaded SAAD Board to invest more in SAAD Digest. Dr Nigel Robb, became the Editor of SAAD Digest and revitalised the societies journal starting a renewal that strengthened into the 2020’s. In April 2006 SAAD launched its RA machine loan scheme in conjunction with Cestradent McKesson, a historic manufacturer of dental anaesthetic and sedation machines. Designed to facilitate the use of inhalation sedation, it offers SAAD members the opportunity to trial inhalation sedation and scavenging systems for a six-month period – along with advice and support – with the option to purchase at a discount rate at the end of this time. This initiative was led by Dr Steven Jones and Dr Derek Debuse. The early 2000s were a period of great innovation for SAAD in terms of its education and training provision, in part as a response to concerns about financial surpluses that conflicted with the Society’s status as a registered charity. One resultant development was a SAAD-endowed Chair in Anxiety and Pain Control for Dentistry based at King’s College London Dental Institute, a position that was occupied by the eminent Washington-based paediatric dentist Professor Peter Milgrom from 2006–2012. At the end of his term working alongside Dr David Craig and his colleagues at King’s, Professor Milgrom reflected on his experience in an article for Volume 29 of Digest: “During the period of my Visiting Professorship, I made wonderful twice per year visits, usually staying in a tiny garret at Goodenough College in Mecklenburgh Square, becoming expert at using my Oyster and learning about the Tube and the buses, and attempting to master a new dialect of the language I thought I spoke well. I gained lots of experience with overcoats and umbrellas, which is saying something for someone from rainy Seattle. I brought to this position experience both with pharmacological and psychological approaches to patients with dental anxiety and avoidance. David (Craig) asked me to offer tutorials for the Diploma and MSc students on behavioural aspect s of dental fears to enrich the in-depth experiences of the students with the pharmacological approaches used in Dentistry. I particularly recall the shock of a couple of students when I asked them to give me an inferior dental block so we could talk about how best to approach patients about this. These students did especially well.” Research grants of up to £5000 were also offered from 2006 onwards, and SAAD funded the research of a PhD student, Joe Hulin, from 2003 – 2016. The results of this research, which explored the decisional needs of young patients, were published in a paper that appeared in Volume 33 of SAAD Digest. This concluded that: “The decision to undergo dental treatment with sedation or GA is a complex healthcare decision and warrants additional decisional support for both patients and their parents/ guardians.” Nigel Robb was elected to the SAAD Presidency having previously served as roles as President of the Association of Dental Anaesthetists and European Federation for the Advancement of Anaesthesia in Dentistry and Chairman of the Dental Sedation Teachers Group The first two years of his presidency were notable for the continuing fallout from the Global Financial Crisis in 2008. The value of SAAD’s assets was affected, and SAAD had to carefully manage our resources during that time. SAAD’s Treasurer, Steve Jones, put in sterling efforts to guide us through this period and enable the society to move forward to introduce many of initiatives that are now part of the life of SAAD. The NICE guidance for sedation in children was produced during this time, and SAAD coordinated a robust response to the consultation. SAAD was involved in theIntercollegiate Advisory Committee for Sedation In Dentistry, IACSD from its outset. Whilst the first incarnation failed and had to be disbanded, the Independent Expert Group for Training and Standards for Sedation in Dentistry was established and published three seminal documents: These three documents were used by the reincarnation of IACSD and the contents were included virtually unchanged in the IACSD standards. SAAD went on to run two advanced sedation techniques courses following on from the production of the syllabi proving that it is possible to deliver this training. To bridge one of the barriers to starting sedation practice, the SAAD Inhalation Sedation Machine Loan Scheme was introduced. This has proved successful in helping many who have completed our National Course introduce Inhalation Sedation to their practices. The General Dental Council changed the Scope of Practice for Dental Hygienists and Therapists to allow them to undertake Inhalation Sedation if they had received the appropriate post registration training. SAAD took a leading role in the development of a course for these groups. This was the first time that SAAD undertook not only to deliver the didactic training, but also to verify the logbooks of students to confirm that they had completed their supervised clinical practice. This experience was hugely helpful when it came to having to apply for STAC accreditation. Nigel led this part of the course until he left for Australia in 2018. In the 2013 edition of Digest, Nigel led the introduction of the online CPD that has become a popular feature with the membership and continues to grow in the number of submissions from members and non-members. The Society continued to seek to extend its reach in subsequent years, and under the presidency of Dr Carole Boyle (2012-2015), free membership of SAAD was offered to all UK undergraduate dental students, along with reduced rates for the symposium and online access to SAAD Digest. The funding of a PhD by SAAD was Carole Boyle’s idea, and she led the proper dissemination of SAAD’s surplus funds back into educational initiatives encouraging research that enhanced the society’s professional standing. Carole Boyle promoted a much-needed change in the society bringing the contribution of women to the forefront. This widened SAAD’s teaching faculty and Board membership. As president 2015-2018 Dr Francis Collier led SAAD through our 60th Anniversary year in 2017. In recent years SAAD had held Board dinners in the RAF Club in Piccadilly. The platinum anniversary dinner was well attended with numerous past presidents and guests who had contributed to SAAD over our last six decades. Dr Steve Jones was inaugurated as SAAD President. After being Honorary Treasurer for thirteen years in 2018 Dr Steve Jones assumed the presidency. His tenure was marked by a “steadying of the ship” following some years of change. Instigating a membership survey Steven Jones decided to pilot an annual symposium outside London and the event was held in Manchester in 2019. By 2020 Steve Jones had to lead SAAD through the world changing events of national lockdowns and restricted professional and social meetings. As COVID 19 changed SAAD’s educational offering and the SSPS scheme was suspended a calm approach was required to guide the society. The challenges of continuing education remotely presented the Board with logistical problems not seen before and Steve achieved cohesion at a difficult time. By 2021 the annual symposium returned to The Royal Society of Medicine. The world had changed but members still wanted to meet and the symposium attracted over 200 members. Dr Sadie Hughes became SAAD’s third female president. SAAD had in early years been a male dominated organisation. Dr Diana Terry and Dr Carole Boyle did much to redress this balance during their presidencies. By 2021 the society had matured, and Sadie Hughes led a more plural Board. By the time Dr Sadie Hughes assumed the presidency a new virtual world had become the norm, and the annual symposium was cancelled. The board of trustees continued to meet virtually and along with paediatric and anaesthetic colleagues, advised the sedation world on the safety of sedation in this turbulent time. With the widespread cancellation of general anaesthetic lists, sedation became even more important for those requiring pain and anxiety management for dentistry. Carole Boyle initiated a popular series of winter webinars enabling sedationists to stay in touch and provided much needed CPD and the SAAD National Sedation Courses went from practical to virtual and with the onset of a national lockdown, SAAD Safe Sedation Practice evaluations ceased. A wave of vaccinations was rolled out and with the majority of clinical staff being vaccinated, a decision to resume the symposium in 2021 was made. It was an unexpectedly sentimental feeling to be back at the Royal Society of Medicine on Wimpole Street, to hold the symposium under the cloud of all that had passed, the historic public control measures and the lives that had been lost during the preceding 18 months. Within a short space of time, the teaching world had changed dramatically. Sedation courses are often virtual, with correspondence and dissemination of information, digital. By 2021 SAAD continued to offer practical hands-on teaching as the board felt this produced more confident, safer sedationists.
Christopher Holden
2000

IFDAS 2003


David Craig
2003

2004
2005
Diana Terry
2006


Nigel Robb
2009
Carole Boyle
2012

Francis Collier
2015


Stephen Jones
2018

Sadie Hughes
2021

SAAD produced its first guidance document, Guidelines for Physiological Monitoring of Patients during Dental Anaesthesia or Sedation, in 1986. This was authored jointly by dentists and anaesthetists, combining both academic opinion and the opinion of experienced clinicians in primary and secondary care. From the 2000s, the governance that SAAD developed in combination with The Royal College of Surgeons of England and The Royal College of Anaesthetists led to the further formalisation of standards and ever-closer relations between doctors and dentists. By this point, expected standards of practice concerning staff training, techniques, the management of complications and emergencies, and the overall patient environment were clearly laid down, with SAAD members leading the process of change. Governance subsequently developed in parallel with the various medical specialties until 2013, when the Academy of Medical Royal Colleges Standards and Guidance document set down minimum standards for all medical and dental specialties. As Christopher Holden and Ian Brett emphasised in their paper on the Society’s history delivered to the 60th Anniversary Symposium, “SAAD has now provided representation or individuals with expertise on every major guidance document in the training and provision of dental pain and anxiety control in the last generation.” SAAD currently has representation on IACSD (Intercollegiate Advisory Committee for Sedation in Dentistry), SDCEP (Scottish Dental Clinical Effectiveness Programme), AoMRC (Academy of Medical Royal Colleges), IEGTSSD (Independent Expert Group on Training Standards for Sedation in Dentistry), DSTG (Dental Sedation Teachers’ Group) and IFDAS (International Federation of Dental Anaesthesiology Societies). Given the overlapping membership of these bodies, “cross-representation” tends to be a naturally occurring process; nevertheless, between 1990 and 2017 SAAD had direct or indirect input into 20 documents, sometimes as an invited member of the group tasked with producing the document, and sometimes via less formal connections. Since its inception SAAD had been heavily involved in deliberations about the regulation of the dental profession in general anaesthesia, conscious sedation, and resuscitation. In 1971 the government proposed a ban on the operator anaesthetist in dentistry. The effect of this would have been to have abolished provision of the intermittent methohexitone technique on which SAAD's teaching was based at the time. Although not promoted by SAAD the operator anaesthetist was a necessity of the time due to the general lack of services of a separate anaesthetist in general dental practice. Patients faced being denied a safe and effective pain and anxiety control technique based on prejudiced opinion in the Ministry of Health at the time. Along with the British Dental Association, SAAD took on the government. A booklet entitled "Treachery" was sent to every Member of Parliament detailing both the sacrifice of basic rights of patients and professional freedom of doctors and dentists and the potential loss of invaluable years of progress in pain control. Members of Parliament agreed - SAAD and the BDA won. Regulation of general anaesthesia had always been a big issue within the General Dental Council. Although there was little genuine experience amongst its own members, it was fortuitous that there was almost always a member of SAAD Council on the General Dental Council. This was important as regulation of anaesthesia, conscious sedation and resuscitation were always closely connected and issues on which the General Dental Council made frequent recommendations. Early in SAAD’s history successive Presidents of SAAD including Dr Gerry Holden, Dr Peter Sykes, and Lord Colwyn a Conservative peer, all contributed to maintaining a sensible but safely directed balance of opinion in relation to the regulation of pain and anxiety. Lord Colwyn provided an important link to government during a politically difficult time for anaesthesia and sedation in dentistry. The definition of conscious sedation drafted by Dr Gerry Holden and Professor Paul Bramley of Sheffield University for the Wylie Report in 1978 was subsequently adopted by the General Dental Council and today remains almost unchanged as the accepted definition of conscious sedation by all UK regulatory bodies. The foundations of SAAD's interest in starting to proactively develop clinical guidelines began in 1989 with the publication in early 1990 of "Guidelines for Physiological Monitoring of Patients During General Anaesthesia or Sedation", led by Dr Peter Cole. This document was well ahead of its time. It heralded SAAD’s drive for proper standards in education and service provision that cemented the societies position in the profession as a trusted teaching and standard setter. This document was occasionally to the irritation of the “academic authorities” but clearly supported by the profession at large. In the 1990s a Department of Health sponsored a guidance document on anaesthesia sedation and resuscitation and published "The Poswillo Report". Dr Peter Sykes and Dr David Phillips were influential in stopping the General Dental Council's attempted knee jerk reaction when it considered banning general anaesthesia for dentistry in primary care at a stroke and almost taking conscious sedation with it. From the early 1990s to this day SAAD has been heavily involved in the production of national guidelines, with representation on nearly every major report concerning anaesthesia, sedation, and resuscitation in dentistry. Particularly active in this area was Dr David Craig, consultant and Head of Sedation and Special Care Dentistry at Guy's Hospital and Dr Christopher Holden, a general practitioner from Derbyshire. A plethora of guidance occurred in the 1990's due to a few heavily publicised and largely unnecessary deaths associated with general anaesthesia and sedation for dentistry. SAAD was quick to realise that the profession needed a guidance document detailing expected standards, but the Society also took the view that this needed to be guidance which involved all parties interested in the subject. In 2000 Dr Christopher Holden chaired an Independent Working Party which ultimately produced a report "Standards in Conscious Sedation for Dentistry" the first standards document for conscious sedation in dentistry. This was later taken forward to a further two documents by a joint committee of the Royal College of Surgeons of England and the Royal College of Anaesthetists. From this standards initiative SAAD played a key role in the production of "Conscious Sedation and the Provision of Dental Care" (Department of Health) in 2003 and "Standards in Conscious Sedation in Dentistry: Alternative Techniques in 2007" (Royal College of Surgeons of England / Royal College of Anaesthetists. At the same time Dr David Craig chaired a report for the Department of Health/Faculty of General Dental Practice (Royal College of Surgeons of England) issuing guidelines for the appointment of dentists with special interest in conscious sedation, importantly providing quality control for NHS Primary Care services. Following several deaths in dental practices, the Department of Health charged Professor David Poswillo, a New Zealand maxillo-facial surgeon, with chairing a working party on anaesthesia, sedation, and resuscitation in dentistry. SAAD had considerable influence in this watershed report, the outcome of which was the development of centres for general anaesthesia and £9 million in government grants to facilities for the purchase of new sedation equipment and staff training. As Dr David Craig commented, “The resuscitation section of the report was less well-received but opened up a productive discussion which led eventually to more practical guidance.” SAAD’s Standards in Conscious Sedation for Dentistry was one of the first standards documents in dentistry. Dr Christopher Holden who chaired the working group commented “Conceptually it was derived from the formulaic use by lawyers of steps necessary to be taken and incumbent on an individual in proper behaviour.” The document was surprisingly well-received, and accepted by the profession, regulators, and government. SAAD’s document quickly stimulated the Department of Health to produce its own document, “A Conscious Decision”, which was essentially an extended version of SAAD’s guidance. The DoH’s document discouraged general anaesthesia for dental treatment and limited it to provision in a hospital setting, a ruling that came into force on 31 December 2001. It encouraged high standards of conscious sedation, including the support of dedicated assistants; appropriate undergraduate and postgraduate training; and arrangements for patient assessment, consent, and patient escorts like those for general anaesthesia. It also called for the availability of better audit data on fatal and non-fatal complications of general anaesthesia and conscious sedation during dental treatment. The latter was still not achieved by 2021. SAAD had a number of contributory authors to this document, which was commissioned by the Department of Health. It defined best practice for conscious sedation for the next 12 years - that is, until the publication of the IACSD Standards in 2015 - and focussed on education and training and the expectation of robust inspection systems. As with earlier documents, SAAD succeeded in moderating the demands of those who wished to see the provision of sedation offered by dentists restricted. However, the document failed to address safety issues associated with multi-drug sedation, the use of which appeared to have increased following the banning of general anaesthesia in non-hospital settings two years previously. This document addressed the on-going concerns of both the Chief Medical Officer and Chief Dental Officer about the use of multi-drug sedation techniques, particularly for young children. It also introduced the concept of “Standard” and “Alternative” conscious sedation techniques (later renamed “Basic” and “Advanced” techniques). The intention was that it would supplement the 2003 DoH guidelines but, as Dr Christopher Holden comments, “Much time was spent refereeing the disagreements between dentists and medically-trained doctors about acceptable techniques.” Although “binding” about dental sedationists, some medical practitioners considered themselves exempt from its guidance. New, and in retrospect, unhelpful terminology complicated the final document, which the profession took some time to accept. Characterised by some as disappointingly the least effective document SAAD has been associated with, being largely ignored by political masters, nevertheless elements of SAAD’s recommendations were developed over the next few years, particularly in relation to the concept of tiering basic and advanced sedation services in service provision. {accirdion title="A Basis for Nationally Structured Guidance"} At last pathways for training, converging specialty agreement and a minimum standard was agreed and accepted by the medical professions. Three documents providing overarching guidance from the Academy of Medical Royal Colleges, Standards from the Intercollegiate Advisory Committee for Sedation in Dentistry, and implementation guidance form the Scottish Clinical Effectiveness Programme. SAAD’s input was instrumental into achieving this. This “umbrella” standards and guidance document had an impact on all medical and dental practitioners, laying down the lowest common denominator for standards in all specialities. SAAD’s input largely defined the direction of this document as other specialties converged on its teaching methods and safety controls. Christopher Holden concludes, “For the first time, it seems it was accepted by all specialties that dentistry not only had its house in order but led the provision of conscious sedation for medical interventions.” This document, which was the successor to the 2013 AoMRC document, defined the practice of dental conscious sedation in the UK. The IACSD Standards were written by a committee which included representatives of the Dental Faculties of the Surgical Royal Colleges, The Royal College of Anaesthetists, and the Dental Sedation Teachers’ Group. Three members of SAAD were involved - David Craig, Nigel Robb, and Christopher Holden. It covered, amongst other things, guidance on clinical techniques, training, the sedation environment, and patient information. An updated version of SAAD’s own Safe Sedation Practice Scheme was intentionally published on the same day as the IACSD document, and its extent, aims and rationale outlined in SAAD’s 2015 Spring newsletter: Evaluation by a peer review process or alternatively self-reflection, contributes to patient safety and reduced morbidity. This scheme is a quality assurance programme aiming to promote a consistent approach which can be applied in any environment providing conscious sedation for dentistry in either primary or secondary care. Earlier versions of the scheme centred around a checklist of mandatory or recommended fields. The 2015 version investigates the patient journey in more depth. There is greater emphasis on assessment and patient centric issues whilst core clinical provision is investigated in detail. […] Fundamentally, this is a practical document which is intended to support and encourage sedation practitioners to meet the contemporary national standards. This document was commissioned in response to the concerns of a minority about a “lack of clarity” in certain areas of the IACSD Standards, together with a feeling that the Standards themselves were not “evidence based”. In an overview of the Review, Dr David Craig concluded that: The new SDCEP Guideline is clear and well written but due to its concise style it lacks some of the breadth and depth of the IACSD Standards. It is also heavily dependent on the IACSD report, especially in relation to multi-drug sedation, training, and patient information. The SDCEP group found no new evidence relating to any of the areas about which concern had been expressed in the IACSD Standards. The SDCEP Guideline fails to resolve any of the contentious issues on which IACSD had struggled to reach unanimous agreement, for example pre-sedation starvation. SDCEP’s Guideline is most likely to be of help to practitioners using “Basic” conscious sedation techniques (intravenous, oral, and intranasal midazolam or inhaled nitrous oxide/oxygen) for straightforward patients in a primary care setting. This politically significant document drew together recent AoMRC, IACSD and SDCEP guidelines to offer guidance to NHS England commissioners. It also defined the process for the accreditation of sedation training courses for dental and medical sedationists and DCPs by the Sedation Training Accreditation Committee (STAC). SAAD Training Board members made a significant contribution to this work.
Guidance Regulation Standards and Politics
There was a proliferation of guidance until 2021 to meet the challenges of robust patient safety and political need. The prominent documents over the years were:
General Anaesthesia, Sedation and Resuscitation in Dentistry ('Poswillo')
1990
Standards in Conscious Sedation for Dentistry (SAAD) A Conscious Decision (DoH)
2000
(DoH), 2002 Conscious Sedation in the Provision of Dental Care
2003
Standards for Conscious Sedation in Dentistry: Alternative Techniques (RCS/RCA)
2007
Framework for Commissioning Sedation Guidance (SAAD)
2013

Safe Sedation for Healthcare Procedures (AoMRC)
2013
Conscious Sedation in the Provision of Dental Care (IACSD)
2015, 2020
Conscious Sedation in Dentistry (SDCEP)
2017
Service Standards for Conscious Sedation (NHS England)
2017