Please click on the tables and figures to enlarge
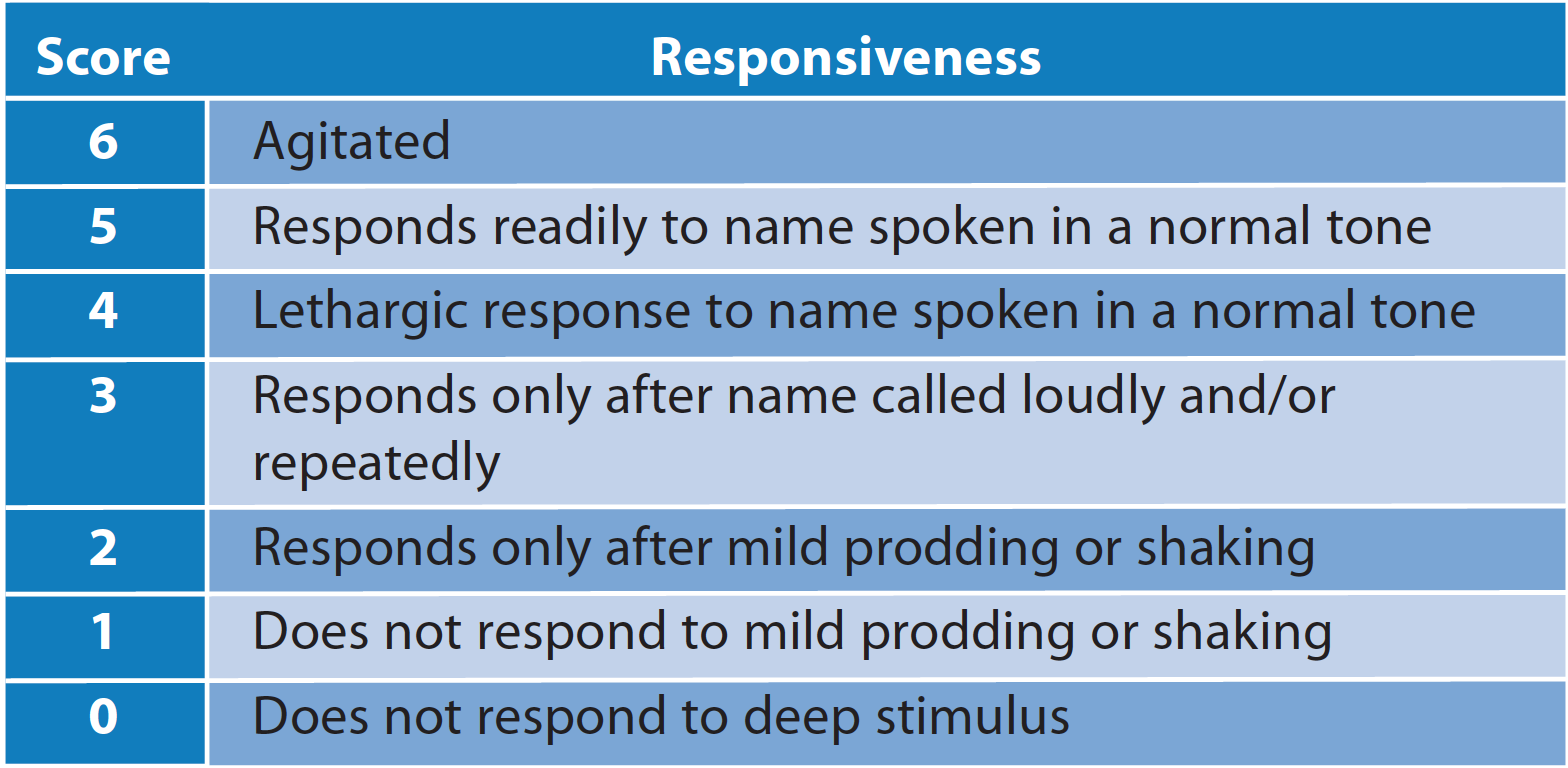
Exploring the environmental impact of the NHS dental service with a focus on conscious sedation and anaesthesia
B. Revert*
Speciality Doctor in Restorative Dentistry, Croydon University Hospital, 530 London Rd, Thornton Heath CR7 7YE
*Correspondence to: Dr Bethany Revert
Email: Bethany.revert@nhs.net
Revert B. Exploring the environmental impact of the NHS dental service with a focus on conscious sedation and anaesthesia. SAAD Dig. 2024: 40(II): 105-109
Abstract
Understanding the extent to which our health service contributes to the climate crisis is vital. All areas of healthcare are currently environmentally unsustainable due to being highly resource intensive. Undertaking dental treatment in both primary and secondary care contributes to the carbon footprint of our health service. This comprises the use of pharmacological intervention with both conscious sedation and general anaesthesia. This paper aims to analyse how we can continue excellent patient care while being more sustainably aware.
Introduction
Over the years, the narrative surrounding climate change has evolved and is becoming widely viewed as the biggest global health threat of the 21st century.1 The principles of beneficence and non-maleficence which underpin dental practice raise an important question: ‘How can we provide dental care without harming the environment and in turn protect our patients?’
Emerging studies have identified an increase in mental ill health and anxiety since the COVID-19 pandemic.2 The need for anxiety management within both primary and secondary care settings has never been more essential but the additional requirements of these patients will increase the carbon footprint of our services. To fully comprehend this impact, evaluation of our healthcare service delivery becomes paramount.
One of the essentials of environmental impact analysis is the quantification of the greenhouse gases. Greenhouse gases are grouped into a common unit called carbon dioxide equivalent (CO2e).3 In 2008, the UK Climate Change Act set out a legal framework to cut gas emissions to 100% below 1990 levels by 2050. This highlighted the need for collaborative effort to ensure positive and productive change to reduce the environmental footprint. High figures for CO2e and waste generation suggest that healthcare delivery is currently not environmentally, socially or financially sustainable.4 To tackle this, the NHS published a report in 2020 providing an updated account of the latest NHS carbon footprint. This report includes an ambition to achieve a ‘net zero’ health service and the initial aim is to reduce greenhouse gas emissions by 80% before 2040. Not only is this an enormous target, but the NHS was the first health service in the world to propose this.5
Most emissions from the NHS fall into three main categories: direct emissions from on-site healthcare, indirect emissions from the generation of purchased energy and indirect emissions due to producing and transporting goods. Areas of healthcare that fall outside of these main categories include staff and patient travel and the carbon footprint of prescribed medication.5
Accurately quantifying the carbon footprint of dental services is challenging. However, it is suggested that 3% of the overall carbon footprint of the NHS in England is due to dental services, which equates to a total carbon footprint of around 670,000 people.6,7
Within the 2021 Lancet report on health and climate change, it was stated that current global commitments are insufficient. They estimated that with no changes we will see a 2.4°C global temperature increase by the end of the century. If the global temperature were to rise above 2°C this would lead to worldwide consequences, including death due to intense heat, alterations in food availability and increased infectious disease transmission.8
Dentistry as a whole
With the joint pressure of the NHS Net Zero target and the Climate Change Act, dentistry within the UK has had to further investigate its role in reducing our carbon footprint. In January 2023, clinical guidelines for environmental sustainability in dentistry were published. These were the first dentistry-focused guidelines relating to improving the sustainability of our profession. The overall aim of these guidelines is to raise awareness, provide needed direction to the dental cohort and to reduce carbon emissions.9 These guidelines incorporate the 2030 United Nations (UN) sustainable development goals, which emphasise the need to ‘take urgent action to combat climate change’.10
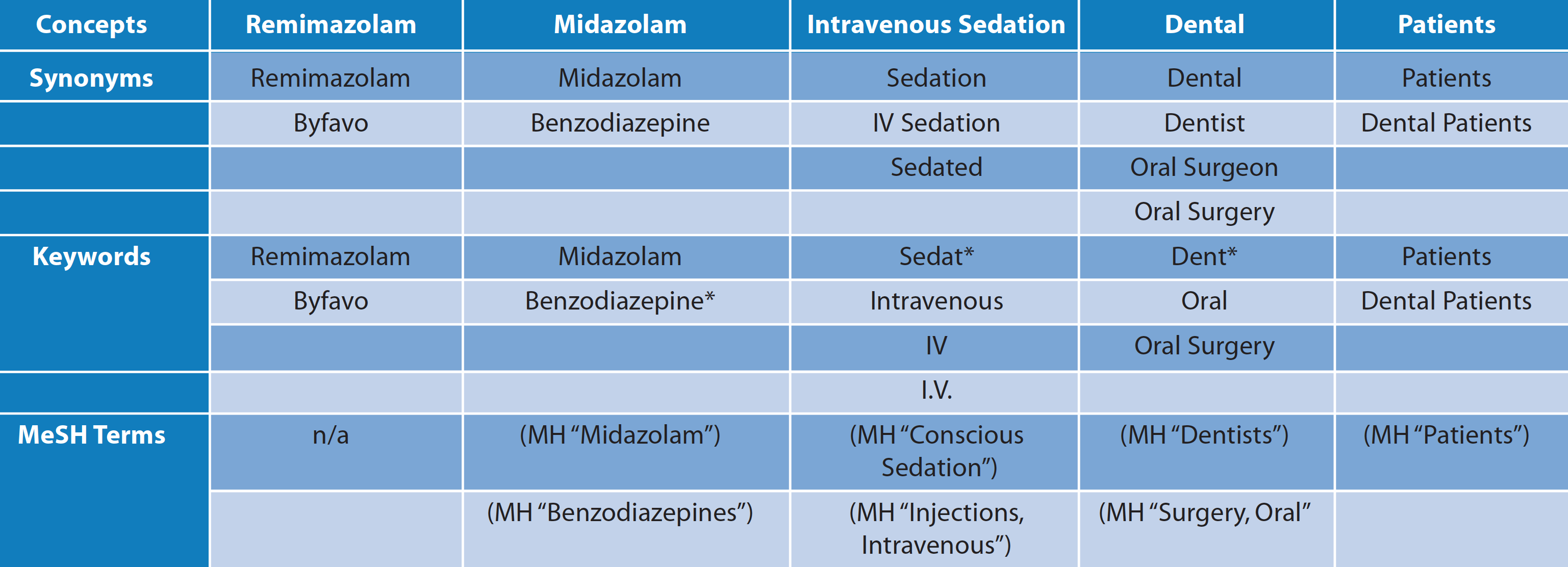
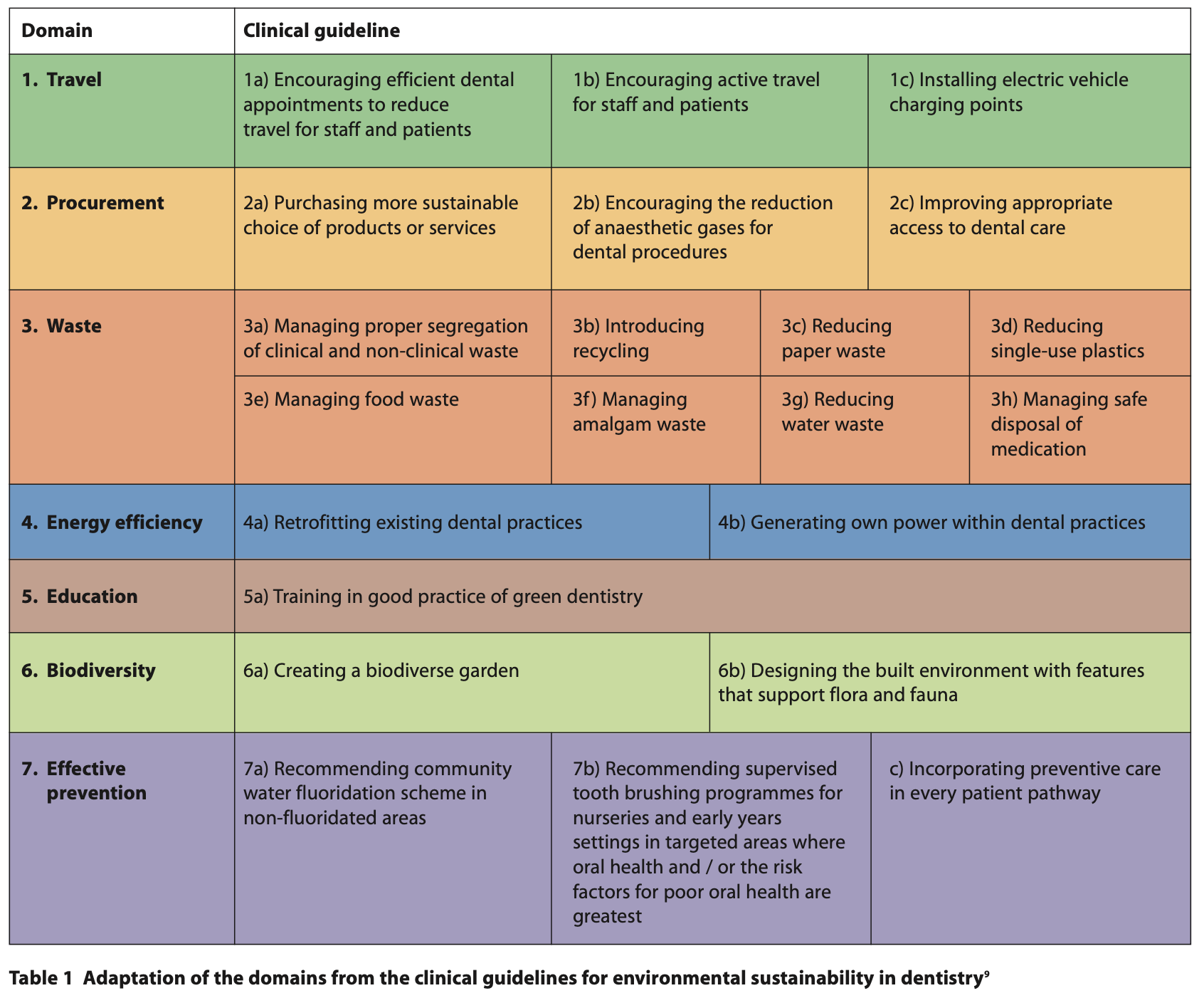
Within the clinical guidelines are seven major domains, which can be seen below in Table 1. Each of these breaks down the multiple facets that lead to the overall carbon footprint within dentistry in England. These guidelines are relevant for individual practitioners, governments and public health professionals. Domain two directly mentions the reduction of anaesthetic gases for dental procedures.9
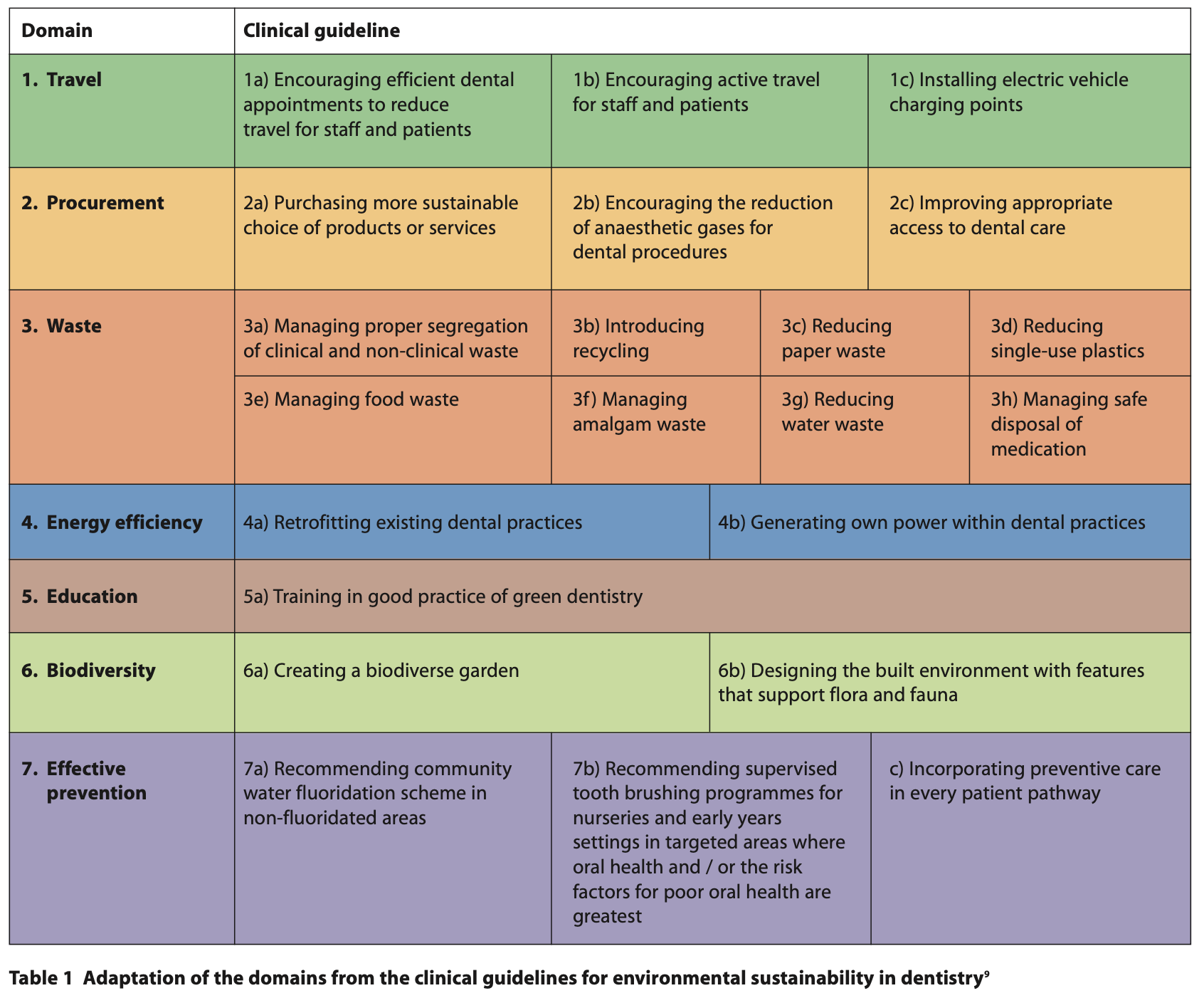
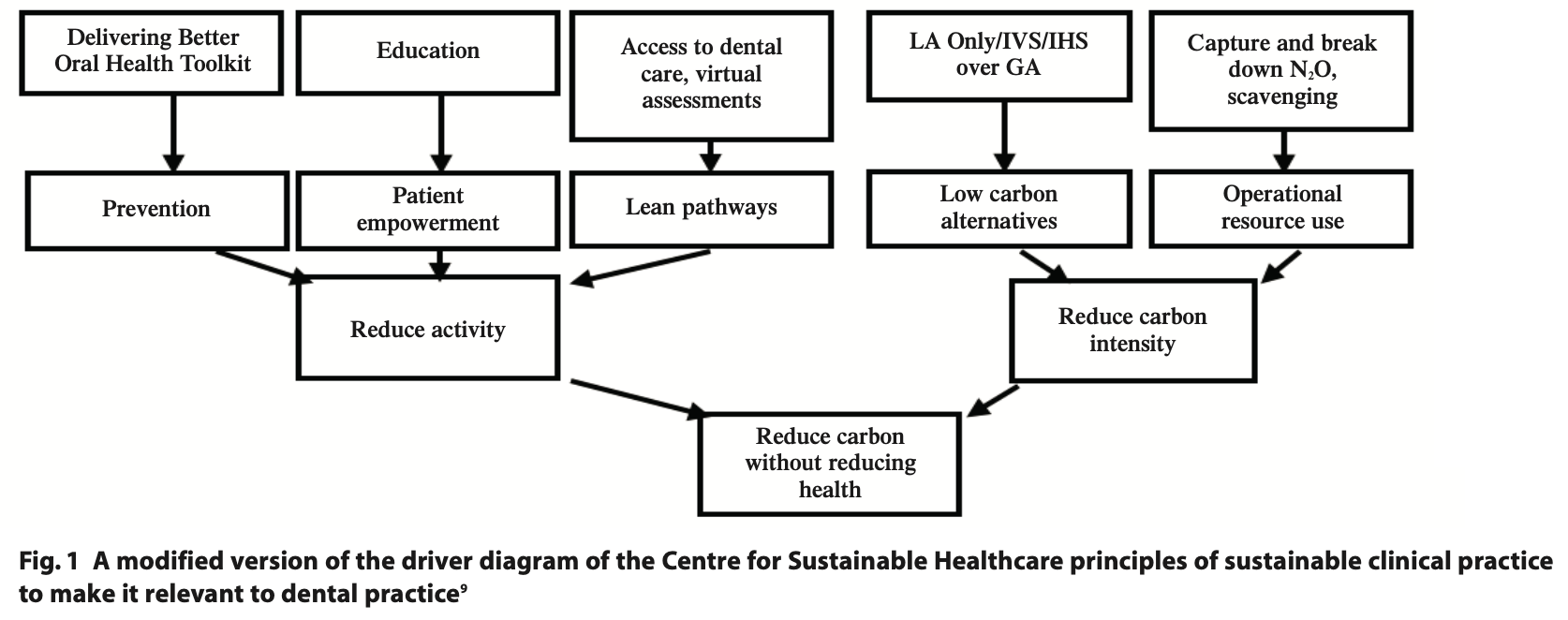
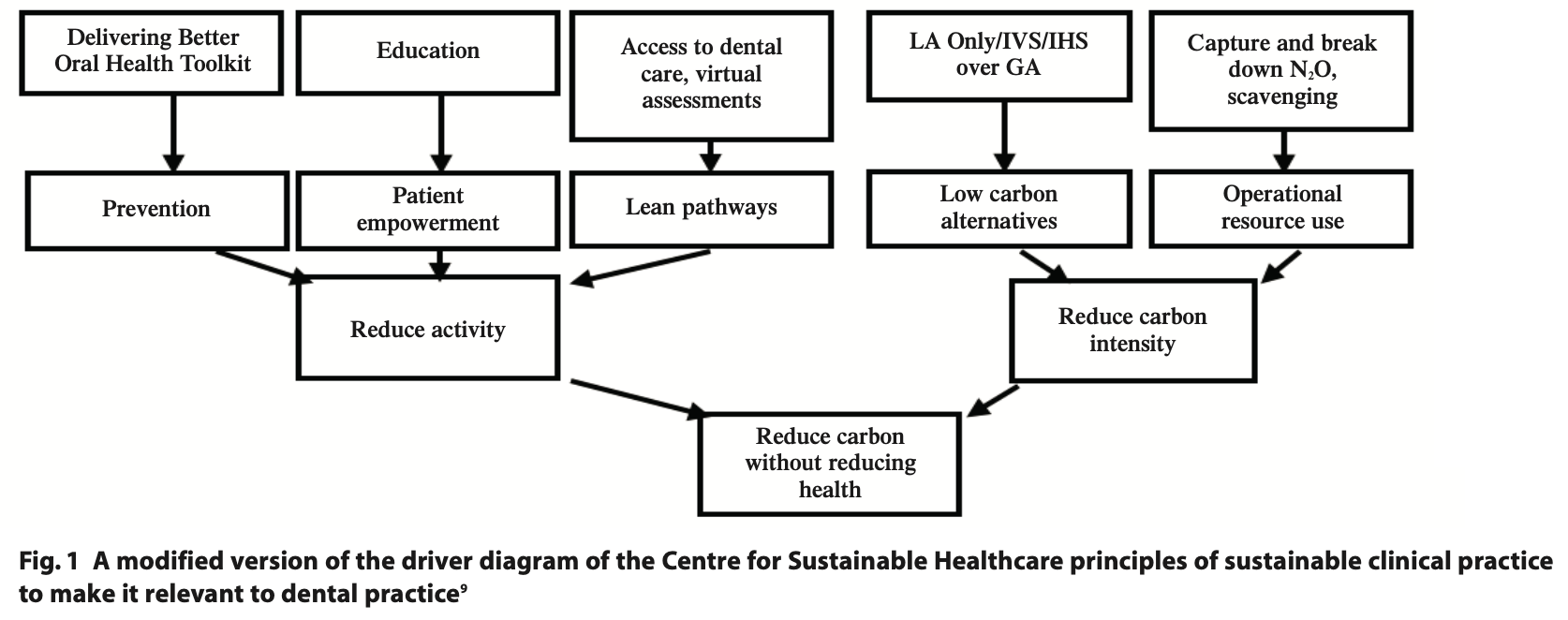
Another useful tool is the Campaign for Greener Healthcare’s four principles. These include underpinning sustainable practice, including disease prevention and health promotion, patient education and empowerment, lean service delivery and preferential use of treatment with a lower environmental impact.11 These areas of improvement can be seen illustrated in the driver diagram in Figure 1.
To be able to reduce carbon intensity, we must investigate which procedures have the largest carbon footprint. Examinations, scale and polishes, radiographs and fluoride varnish applications have the lowest carbon footprint due to the minimal materials used. However, due to the extensive number of examinations required, it still equates to a large proportion of our carbon footprint. Procedures with higher carbon footprints come from more extensive procedures, which either require increased material use or multiple appointments. In clinical situations where conscious sedation or general anaesthesia (GA) is required, an increased carbon footprint occurs due to the addition of more staff and the use of N2O or other gases.7
The most used dental materials are amalgam and composite. Excluding the presence of mercury within amalgam, the comparative carbon footprint of these two materials is unknown. In addition, the environmental breakdown of these products is not understood. Motivation for these analyses to take place is required, allowing the profession and public to make an informed material choice. However, it is known that dental mercury equates to 3 - 4% of terrestrial mercury. In total 75 metric tonnes of amalgam are used per year in the EU alone.3 The Minamata Convention has highlighted the need to reduce mercury use across the globe, which has directly impacted usage in dentistry. Conversely, in clinical situations where moisture control is difficult to achieve or when applying the most affordable option, amalgam is still a material of choice.12
Although looking at dental procedures and materials is important, we know that the highest proportion of emissions due to dentistry in the UK came from travel, procurement, energy and N2O.7 Therefore, further analysis of indirect carbon usage in dentistry needs to be completed. Approximately 3.5% of all road travel in England is due to healthcare-related excursions.5 Despite it being an indirect cause, encouraging staff and patients to switch to lower carbon footprint transport options is essential. Alongside this, we can evaluate the patient pathway by highlighting access to dental services. NHS England is required to ensure it commissions services in areas that are easily accessible for patients to travel to and from, as well as being available to all.7 Timely diagnosis and treatment, can minimise the need for further invasive treatment. There is a delicate undertaking with this, as more practices also add to increased output and a higher carbon footprint.
In the same way that access is important, we must also explore how an integrated care model could improve our carbon footprint.13 Certain areas of the UK don’t have facilities for dental treatment under sedation, therefore in some circumstances, GA may be the only option for these patients. GA requires more staff and increased use of ozone-depleting gases. Therefore, if it was possible to design and deliver more efficient, effective patient pathways we could reduce the need for unnecessary high carbon footprint procedures.
To tackle both travel and the use of resources, one suggestion to make dentistry more sustainable is to complete as much treatment in one session as possible. However, when pharmacological intervention is required due to dental anxiety or medical history, there is a limiting factor of drug working time. Whilst this may be more achievable under GA, this is not necessarily the most practical or safe option due to theatre availability and the risks of anaesthesia. Furthermore, GA itself carries a heavy carbon burden through travel, staffing, enormous waste generation and energy consumption.14
Before using pharmacological interventions, all steps should be taken to try the least invasive option. This can include acclimatisation of dental treatment. If this is not possible due to severe anxiety, an appropriate pre-assessment should be completed. This includes an anxiety assessment tool, such as the Modified Dental Anxiety Scale.15 Patients are required to reach a certain threshold to qualify for sedation techniques under our current health service. This is a useful tool in ensuring we are only undertaking appropriate treatment measures. To reduce the environmental impact of sedation even further, reducing the prevalence of dental anxiety is required. Ideally, the use of psychotherapeutic interventions should be first-line management before pharmacological agents. However, in patients with severe anxiety, a combination of both may be required. The use of these additional psychological interventions could lead to a patient being able to undergo dental treatment without conscious sedation thereby improving patient outcomes, whilst reducing the environmental footprint as a side effect.16
Inhalation sedation with N2O
In current dental practice inhalation sedation (IHS) is undertaken inboth primary and secondary care settings. Indications for its use include dental anxiety, needle-phobia, traumatic or prolonged dental procedures, medical conditions aggravated by stress and patients who require sedation and who have no escort.17
In dentistry, we regularly use nitrous oxide (N2O) for conscious sedation which is a potent greenhouse gas. The global warming potential (GWP) of N2O is 298 times higher than CO2. Despite it having a shorter life cycle than CO2, the damage it causes within the same timeframe is much increased.18 The N2O released during the sedation of an estimated 63,749 patients, produced almost 1% of the total carbon footprint of NHS dental services in England.8
In dental practice, the exhaled gas is removed using a scavenging system. This delivers the exhaled vapours out of the clinical environment, which aims to reduce the occupational exposure of staff. It is common practice to also ensure adequate fitting of the nasal hood to ensure no excess N2O is released into the local environment.7 However, N2O does not undergo any form of metabolic change within the human body, and therefore any exhaled gas will pollute the planet.3 Suitable alternatives to releasing this exhaled N2O are being explored. Technological advances are being trialled, mainly within theatre settings in the UK, though European counterparts have already been using N2O denaturing devices for several years.
Despite N2O’s high GWP the use of IHS is seen as a less invasive option compared to intravenous sedation (IVS) or GA. Therefore, there is a delicate balance between minimising the use of IHS while still offering the least invasive treatment option.7
General anaesthesia using ozone-depleting gases
It has been estimated that an average of 163 litres of N2O is used during one procedure of GA per patient episode. This does not consider the carbon footprint of the travel and procurement process.3 The use of inhalational anaesthetic agents equates to around 5% of the total carbon footprint of acute NHS trusts. It is therefore unsurprising that when N2O is used, it equates to the biggest component of the carbon footprint of GA.19
Steps can be taken to reduce the amount of N2O used during GA. These include ensuring well-fitting masks, flushing of the system correctly, turning off valves as soon as no longer required and ensuring there are no leaks within the system.3
The use of catalytic splitting could cut over one-third of NHS anaesthetic emissions.5 This process requires an external unit to heat the N2O to 400°C, producing both oxygen and nitrogen as by-products. This technology has been successfully deployed in Sweden.20 Currently this is more readily used for GA due to the ease of installing one large unit for multiple theatres. However, we are starting to see the use of smaller units in dental settings for single rooms. For example, Medclair has produced a mobile destruction unit which reduces over 99% of N2O to its harmless byproducts.21 This is currently being piloted in England to investigate the ease of use for dental services. Promising results have been seen with this technology, for example a 52% decrease in N2O emissions from birthing units in Stockholm.20
As healthcare professionals, we already aim to try and avoid the need for GA due to additional medical risks. The knowledge of the increased environmental impact of GA allows us to further warrant the use of less invasive means. Due to the recent COVID-19 pandemic, waiting lists for GA suites are high and ever-growing,22 therefore further funding is required to allow the implementation of such technologies to offset the high use of theatres.
Sedation using midazolam and alternatives
Where IHS is contraindicated or anxiety management is unsuccessful, alternative pharmacological interventions can be applied. One of the most common options is the use of midazolam. The route of delivery for this drug can be either intranasal, oral or intravenous. Generally intranasal and oral routes are used pre-operatively before completing cannulation for intravenous midazolam use.23
Compared to non-sedation related practices, we can be certain the carbon footprint of the additional drug and environmental impact for disposal will be greater. However, comparing IVS directly to inhalation practice is more complex. It has been suggested that total intravenous anaesthesia could have a lower environmental impact, it also reduces the risk of occupational exposure and pollution to the atmosphere. Despite this, correct disposal of all IV agents should be followed to reduce environmental contamination.24 This evidence could be applied to IVS, however, within dentistry this is seen as the more invasive option over IHS. This is due to the prolonged recovery period, the requirement for an escort and the additional monitoring required. Therefore, despite the possible reduced carbon footprint, we are unable to ethically suggest the use of intravenous midazolam over IHS.
In certain situations, for example severe dental anxiety or low co-operation, midazolam can be administered alongside other agents or alternative agents used entirely. These include fentanyl, propofol, ketamine and sevoflurane gas.23 Sevoflurane is less environmentally damaging compared to N2O and it is comparable for sedation, but further research and adaptation to dentistry is required before routine use.25
Like midazolam there is limited evidence on the environmental impact of fentanyl, propofol and ketamine use for dentistry. These drugs are used as advanced techniques and are likely occurring in small numbers.23 Further research is required to fully understand the breakdown of these products in the ecosystem.
Clinician education
A recent study showed that only 9% of students believed they had formal teaching on sustainability despite 97.3% of students believing the profession should be more actively engaged.26
For many years, the General Medical Council has implemented specific learning outcomes for undergraduates, focusing on sustainable healthcare.27 This was an early sign that interest in the link between our medical practices and the environment was increasing. In November 2023, the General Dental Council launched the new framework for dental professional education, which will be implemented in undergraduate programmes from 2025. This framework includes a sub-domain called social accountability, requiring formal teaching on sustainable oral health and the environmental impacts of common treatment methods.28 This change allows us to engage the future generation of healthcare professionals to enable them to aim for more sustainable practice.
For our postgraduate colleagues, an introductory course on sustainability is available free for all on Health Education England’s e-Learning for Health platform.29,30 Training courses such as this require promotion by local trusts to ensure the workforce is aware of their existence.
Patient education
A downstream, preventative approach to oral health care will have the biggest impact on reducing the need for dental treatment.31 Preventative items such as fluoride toothpaste, fluoride varnish and fissure sealants can reduce the likelihood of large areas of dental caries and therefore restorative treatment.31 Education for care staff or carers can add another layer to the preventative approach. Improving education and knowledge can reduce an individual's likelihood of poor oral health. We must ensure we are following the Delivering better oral health toolkit to assess the risk status of our patients and giving them tailored advice and education.31
COVID-19
During the COVID-19 pandemic, phone triage became the only option for patients who were experiencing dental pain and swelling, and many patients were left without access to treatment.32 Despite national restrictions being lifted there has been a continuation of this practice with some using an initial video assessment before treatment.33 This is a useful tool to mitigate the need for travel for initial discussions or where a clinical exam is not required. This is useful for patients with access or transport difficulties. The long-term implementation of virtual assessments and telephone consultations could help reduce patient travel.
Conclusion
The long-term sustainability of our health service relies on the collaboration and motivation of all specialities. Successfully treating patients with conscious sedation or GA is a clinical necessity and so further research is required to allow us to aim for a more environmentally sustainable practice. Indirect causes of carbon usage such as travel, procurement and wastage require further alteration and motivation from the workforce at all levels. The use of N2O is concerning, although clinically necessary for anxiety management, and advances in catalytic cracking are likely to have the biggest impact on reducing the damage caused by N2O. Downstream prevention of both dental disease and dental anxiety is vital to help reduce the need for treatment, this practice can only be successful with patient and clinician education. In conclusion, we can shape a more sustainable and safe future by collaboratively working together.
Declaration of Interest
There are no conflicts of interest.
Acknowledgements
I would like to acknowledge Dr Zahra Shehabi, for inspiring me to become involved in this area of dentistry, as well as her continued support in my career.
References
1. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet 2009; 373: 1693-1733.
2. Santomauro D F, Herrera A M M, Shadid J et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021; 398: 10312: 1700–1712.
3. Martin N, Sheppard M, Gorasia G P, Arora P, Cooper M, Mulligan S. Awareness and barriers to sustainability in dentistry: A scoping review. J Dent 2021; 112: 103735.
4. Duane B, Stancliffe R, Miller F A, Sherman J, Pasdeki-Clewer E. Sustainability in dentistry: a multifaceted approach needed. J Dent Res 2020; 99: 998-1003.
5. Greener NHS. NHS England and NHS Improvement. Delivering a Net Zero NHS. 2020. Online information available at: https://www.england.nhs.uk/greenernhs/publication/delivering-a-net-zero-national-health-service/ (accessed March 2024).
6. Public Health England. Carbon modelling within dentistry: towards a sustainable future. Crown: London. 2018. Online information available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/724777/Carbon_modelling_within_dentistry.pdf (accessed March 2024).
7. Duane B, Lee M B, White S, Stancliffe R, Steinbach I. An estimated carbon footprint of NHS primary dental care within England. How can dentistry be more environmentally stable? Br Den J 2017; 223: 589-593.
8. Romanello M., McGushin A, Napoli D et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 2021; 398: 1619-1662.
9. Duane B, Fennell-Wells A. 2023. Clinical guidelines for environmental sustainability in dentistry.
10. United Nations DoEaSA, The 17 United Nations Sustainable Development Goals. 2015. Available at: https://sdgs.un.org/goals (accessed March 2024).
11. Mortimer F. The sustainable physician. Clin Med (London) 2010; 10: 110-1
12. Fisher J, Varenne B, Narvaez D, Vickers C. The Minamata Convention and the phase down of dental amalgam. Bulletin of the World Health Organization. 2018; 96: 436–438.
13. Willcocks S, Willcocks E. The shift to integrated care in the NHS: implications of the new care models for dentistry. Br Dent J 2019; 226: 319–322.
14. Shelton C L, McBain S C, Mortimer F, White S M. A new role for anaesthetists in environmentally-sustainable healthcare. Anaesthesia 2019; 74: 1091–1094.
15. Humphris G M, Dyer T A, Robinson P G. The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health. 2009; 9:20.
16. Appukuttan, D. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Investig Dent 2016; 8: 35–50.
17. Coulthard P. The indicator of sedation need (IOSN). Dent Update 2013; 40: 466–471.
18. Erisman J W, Galloway J, Seitzinger S, Bleeker A, Butterback-Bahl K. Reactive nitrogen in the environment and its effect on climate change. Curr Opin Environ Sustain 2011; 3; 81-290.
19. Shelton C L, McBain S C, Mortimer F, White S M. A new role for anaesthetists in environmentally sustainable healthcare. Anaesthesia 2019; 74(9): 1091–1094.
20. Ek M, Tjus K. Destruction of Medical N20 in Sweden. In Greenhouse Gases – Capturing, Utilization and Reduction. pp 187-198. London: IntechOpen, 2012.
21. Medclair. MDU - Mobile Destruction Unit Medclair. 2013. Online information available at: https://www.medclair.com/en/mdu (accessed March 2024).
22. NHS. Delivery plan for tackling the COVID-19 backlog of elective care. 2022. Online information available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2022/02/C1466-delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care.pdf (accessed March 2024).
23. The dental faculties of the Royal Colleges of Surgeons and the Royal College of Anaesthetists. Standards for Conscious Sedation in the Provision of Dental Care (V1.1), Report of the Intercollegiate Advisory Committee for Sedation in Dentistry. 2020. Online information available at: https://www.saad.org.uk/IACSD%202020.pdf (accessed March 2024).
24. Varughese S, Ahmed R. Environmental and Occupational Considerations of Anesthesia: A Narrative Review and Update. Anesth Analg 2021; 133: 826-835.
25. Allen M, Thompson S. An equivalence study comparing nitrous oxide and oxygen with low-dose sevoflurane and oxygen as inhalation sedation agents in dentistry for adults. Br Dent J. 2014; 217: E18–8.
26. Durnall, O., Martin, N., Mulligan, S., Dixon J. Environmental sustainability: the attitudes and experiences of UK students in the oral health care profession. Br Dent J 2024.
27. Duane B, Harford S, Ramasubbu D et al. Environmentally sustainable dentistry: a brief introduction to sustainable concepts within the dental practice. Br Dent J 2019; 226: 292–295.
28. General Dental Council. The Safe Practitioner: A framework of behaviours and outcomes for dental professional education, dentist.2023. Available at: https://www.gdc-uk.org/docs/default-source/safe-practitoner/spf-dentist.pdf?sfvrsn=c198211d_5 (accessed March 2024).
29. Fennell-Wells, Amarantha. The current status of sustainability in dentistry: a perspective. Br Dent J 2023; 234: 245. Doi: 10.1038/s41415-023-5566-6.
31. Public Health England. Delivering better oral health: an evidence-based toolkit for prevention. 2014. Online information available at: https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (accessed March 2022).
32. Hurley S, Neligan M. Letters, updates, and additional guidance for dental teams. 2020. Online information available at: https://www.england.nhs.uk/coronavirus/publication/preparedness-letters-for-dental-care/ (accessed March 2022).
33. Parker K, Chia M. Patient and clinician satisfaction with video consultations in dentistry - part one: patient satisfaction. Br Dent J 2021. Online information available at: https://www.nature.com/articles/s41415-021-3007-y#citeas (accessed March 2024).